Gastroenterologist Our clinics Rectoscopy Ultrasound of the abdominal cavity
Gastroscopy is one of the most informative studies of the stomach, which is difficult to replace with another method. Gastroscopy allows you to examine the mucous membrane from the inside and identify possible changes. If a pathological formation is detected, a biopsy is simultaneously performed - taking a small piece of tissue for histological examination.
Gastroscopy is not always indicated, since this study may cause slight injury to the mucous membrane of the esophagus and stomach, and irritation of the pharynx. The study may cause excessive anxiety and fear in patients, which can cause increased blood pressure and pain in the heart area.
Examination of the gastrointestinal tract using a flexible endoscope
FGDS (gastroscopy)
is one of the options for endoscopic examination, which allows for an external examination of the mucous membranes of the intestines, esophagus and stomach. The procedure is performed using a flexible endoscope equipped with a fiber-optic system, a manipulator and a small video camera. The image transmitted to the monitor screen can be saved in the computer memory as a file.
In addition to photo and video recording, the endoscope allows you to perform the following operations:
- removal of tumors;
- stopping bleeding;
- administration of medications.
Fibrogastroduodenoscopy is performed as prescribed by the treating or consulting doctor. FGDS is used to diagnose gastritis, cancer, duodenal and gastric ulcers, inflammation of the esophageal mucosa and duodenitis. Gastroscopy may be prescribed as an additional procedure to clarify the diagnosis of allergic reactions, pain in the upper abdomen and cardiovascular pathologies.
Indications for FGDS
Due to the wide range of possibilities of the FGDS procedure of the stomach, there is a fairly large list of indications for this medical procedure. The doctor will prescribe an FGDS if you notice the following symptoms:
- Abdominal pain of any location;
- Constant nausea and frequent vomiting;
- Difficulty swallowing;
- Unreasonable fluctuations in body weight;
- Anemia;
- Excruciatingly painful heartburn.
As noted above, FGDS can be used both for diagnostic purposes and as a therapeutic technique. The diagnostic procedure of FGDS of the stomach is the most informative method for determining the following pathologies:
- Gastritis;
- Colitis of various etiologies;
- Stomach ulcer;
- Neoplasms, both malignant and benign;
- Dyskinesia of the gallbladder;
- Esophagitis;
- Duodenitis.
An indication for therapeutic fibrogastroduodenoscopy may be the need to remove polyps and erosions, as well as foreign objects in the stomach. FGDS allows excision of a small area of tissue for microscopic examination and biopsy, which makes it possible to accurately make a diagnosis and develop a competent treatment strategy. In addition, in rare cases, gastroscopy of the stomach may be prescribed on an emergency basis to stop intracavitary bleeding.
Features of the diagnostic procedure
6-8 hours before FGDS, food intake is completely excluded. The examination is performed on an empty stomach. The procedure is carried out in special rooms, operating rooms and intensive care wards. Local or general anesthesia may be used before the examination. The second option is used in case of a pronounced gag reflex, severe anxiety of the patient and the presence of specific diseases (hiatal hernia, Barrett's esophagus, etc.).
The endoscope tube is inserted through a special mouthpiece, which the subject clamps with his teeth. During FGDS, it is necessary to relax and ensure the necessary breathing rhythm (smooth and shallow inhalations and exhalations). During the examination, an air mixture is supplied to the endoscope, with the help of which the cavities of the organs of the upper gastrointestinal tract are straightened. The average duration of fibrogastroduodenoscopy is 5-7 minutes. The diagnostic results are entered into the endoscopic examination protocol.
Relative contraindications to gastroscopy
There are no absolute contraindications to gastroscopy. In other words, there are no conditions that categorically prohibit the conduct of research. There is a group of diseases and characteristics of the human body in which gastroscopy must be postponed for some time. All these conditions are combined under the term relative contraindications.
Contraindications for endoscopic examination of the stomach are divided into groups depending on the organ system to which the disease that caused the delay in the examination belongs:
- cardiovascular
- diseases of the musculoskeletal system and traumatic injuries
- neurological disorders of the central and peripheral nervous system
- metabolic disorders and endocrine pathologies
- blood system diseases
Gastroscopy in the presence of relative contraindications is carried out only after preliminary preparation aimed at relieving pathological conditions.
Contraindications to gastroscopy from the heart and blood vessels:
- decompensated heart failure
- recent myocardial infarction
- diagnosed thoracic or abdominal aortic aneurysm
- frequent attacks of angina pain
- arterial hypertension 3-4 degrees
Contraindications to gastroscopy from the blood system and hematopoietic organs:
- hemophilia
- decrease in blood coagulation factors according to hemogram
- varicose veins of the esophagus
- narrowing of the esophageal opening of the stomach
The entire group of contraindications increases the risk of developing complications such as bleeding.
Anatomical defects of the musculoskeletal system create the prerequisites for difficulties in passing a soft endoscope to the gastric cavity.
When is it necessary to do a gastroscopy?
It is a mistake to underestimate the effectiveness of these two methods in determining a number of diseases. For doctors, they are the main ones in the study of the gastrointestinal tract.
Gastroscopy helps to identify diseases such as:
- peptic ulcer;
- malignant diseases of the esophagus, stomach;
- presence of erosion;
- polyps;
- types of gastritis;
- the presence of foreign bodies and much more.
Most often, a doctor will refer you for a gastroscopy if you complain of stomach pain, frequent heartburn, vomiting, loss of appetite, weight loss, difficulty swallowing and pain associated with eating.
A modern endoscope is able to show the most accurate information about the state of the gastrointestinal tract to the doctor, while the examination is carried out more thoroughly under drug sedation.
The main requirements for the patient during gastroscopy are to limit food intake 10 hours before the examination, as well as abstain from drinking water for three hours.
If the patient needs to take medications on a special schedule, it is worth agreeing with the doctor.
Methodology of the procedure
Planned FGDS is carried out in the morning.
So, the patient is in the gastroscopy room. He was given a sedative, his throat was treated with lidocaine - the patient felt numbness in the tissues of the oral cavity.
The patient is asked to sit on a special table in a position lying on his left side, with a straight back. A mouthpiece is placed in the mouth (to prevent damage to the teeth and probe), through which a flexible gastroscope tube is inserted. The doctor asks the patient to make a swallowing movement and at this moment pushes the probe into the esophagus. This moment is the most unpleasant for the patient, since his gag reflex is triggered. The patient should realize that all unpleasant sensations depend solely on him: he should try to relax as much as possible, suppress the gag reflex, breathe calmly, deeply, through the nose and mouth at the same time.
When the probe enters the esophagus, the specialist begins the inspection process: turns on the video camera located at the end of the endoscope and studies the structure of the mucous membrane on the monitor screen. To examine every centimeter of the mucous membrane, the doctor moves the probe up and down, back and forth, and turns it. If necessary, he takes photos of certain areas or even films the research process on video.
If indicated, tissue samples can be taken during FGDS for further microscopic or other types of examination. Also, without taking out an endoscope, the doctor can coagulate a bleeding vessel, which will stop the bleeding, administer the necessary medications (antibiotics, antiseptics or others) and even remove a tumor (for example, a polyp).
When the examination is completed, the doctor carefully removes the endoscope, helps the patient sit down and after 15-25 minutes allows him to go to the ward (accompanied by medical staff).
The specialist records the results of the FGDS in the patient’s chart, who discusses them with his attending physician.
What does FGDS reveal?
The examination gives an accurate idea of the anatomical structure of the organs, the condition of the mucous membranes of three organs at once: the esophagus, stomach and duodenum. Using an FGDS examination, you can promptly identify the most common diseases of the gastrointestinal tract, namely:
- gastritis;
- stomach and duodenal ulcers;
- erosive lesions of the stomach;
- stomach polyp;
- benign tumors;
- stomach cancer.
Using the procedure, the causes of dysphagia and recurrent vomiting are also determined, the source of bleeding is found, materials are collected for biopsy, and minor surgical interventions are performed (for example, removal of polyps).
FGDS and FCS - an endoscopist of the highest category answers questions
At the Persha Private Polyclinic MC, fibrogastroduodenoscopy (FGDS) is performed comfortably - this is noted by all patients who have previously had to deal with gastroscopy in other institutions. In our work we use a modern gastroscope (OLYMPUS EXERA GIF-160) with an outer diameter of only 8.6 mm. The examination is carried out by an endoscopist of the highest category with extensive experience.
Many patients are wary of FGDS, which is completely normal, because the instincts of any healthy person protest against the ingestion of foreign bodies. However, in many cases it is impossible to do without endoscopic examination.
In order to answer questions that concern many patients who were prescribed FGDS, we interviewed an endoscopist of the highest category, a member of the board of the Ukrainian Association of Endoscopists Oleg Albertovich Fetisov
Esophagogastroduodenoscopy, what is it?
Gastroscopy, fibrogastroscopy, video gastroscopy and other words where “gastro” (stomach) and “skopia” (study) appear mean the study of the stomach, esophagus and duodenum using a flexible optical device - an endoscope. There are many models of such devices - some of them are inserted through the nose.
In what cases is it necessary to perform FGDS?
Here are the main symptoms for which you may be prescribed a test:
- pain in the upper abdomen, located between the navel and the xiphoid process of the sternum (doctors call this area “epigastric”, “epigastric region”), especially if they occur immediately after eating or on an empty stomach;
- constantly bothered by heartburn, sour belching;
- vomiting of undigested food, vomiting with blood, “vomiting like a fountain” (with obstruction of the esophagus);
- a feeling of heaviness and fullness in the stomach, which intensifies immediately after eating.
FGDS is indispensable in the diagnosis of cancer, precancer and chronic inflammatory diseases - the method allows you to detect a pathological focus in time and take appropriate measures. Modern gastroscopes allow you to take a suspicious area of tissue (biopsy) for subsequent study in the laboratory.
When is the FCC needed?
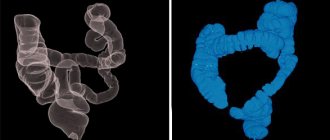
Fibercolonoscopy is an endoscopic examination of the large intestine (a flexible probe as thick as an index finger).
Prescribed for the following conditions:
- intestinal bleeding (red or scarlet blood);
- periodic pain in the lower abdomen;
- loose stool
- suspicion of cancer or polyposis of the large intestine, especially in combination with oncology in direct relatives, the need for a biopsy of the corresponding section of the intestine;
- foreign body in the colon;
- diagnosis and monitoring of conditions in Crohn's disease, nonspecific ulcerative colitis (UC), iron deficiency anemia;
- intestinal obstruction.
After 50 years, FCS must be carried out at least once every 2 years, even in the absence of complaints. Colon cancer very often develops unnoticed, and only with the help of FCS can it be detected in time. At stage 1, the tumor can be removed using an endoscope without incisions and virtually without hospitalization.
Is it possible to replace FGDS with ultrasound or CT?
The use of CT or ultrasound techniques allows only indirect assessment of the condition of the walls of hollow organs (stomach or intestines). These methods are suitable for the diagnosis of foreign bodies, space-occupying tumors and diseases of parenchymal organs (liver, kidneys, spleen), but not for the intestines.
Only an endoscope can show the doctor the real condition of the mucous membrane and make it possible to take tissue from a suspicious area of the intestine, esophagus or stomach. Using an endoscope, the doctor can stop bleeding or remove a polyp that has begun to turn into a malignant tumor.
How long does the study last?
The duration of diagnostic gastroscopy depends on the goals and objectives set for the endoscopist.
The time for a conventional diagnostic gastroscopy largely depends on the experience and skills of the doctor: our study (on average) takes 2-3 minutes.
If you need to take material for cyto-histological examination, the time for gastroscopy increases slightly (depending on the number of mucosal areas that are subject to mandatory histological examination).
A colonoscopy takes 10-15 minutes and also depends on the experience and skills of the endoscopist, as well as the specific clinical situation: the presence of pelvic adhesions or severe inflammatory changes in the colon mucosa increases the examination time to half an hour. In such cases, for the greater comfort of our patients, we recommend conducting the study under anesthesia (FCS in medicated sleep).
Preparation for FGDS
The procedure is carried out on an empty stomach - the stomach and duodenum must be free of food. As a rule, it is enough not to eat or drink anything other than water for 8 hours before the test. Depending on the type of study, recommendations may vary.
It is very important that you tell your doctor about your medical conditions and previous tests.
Preparing for the FCC
The large intestine should be free of contents. To do this, use laxatives or administer large amounts of liquid (enemas). Your doctor will provide detailed instructions for preparing for the FCS.
Is it possible to do gastroscopy in the afternoon or evening?
It is preferable to do it in the morning, since in the afternoon the stomach is filled with secretory fluids, which makes the study difficult. That is why gastroscopy is classified as a “study of the morning hours,” that is, carried out in the first half of the day.
Endoscopists Medical Networks
Nechaev Dmitry Valerievich
Zhuchkova Irina Nailevna
Equipment
View prices
FGDS is a method of endoscopic examination
, thanks to which a detailed examination of the digestive system (more precisely, the esophagus, stomach, duodenum) is carried out. The main goal is a visual examination to identify pathologies and monitor the effectiveness of the treatment. In some cases, during the procedure it is possible and advisable to take material for a biopsy.
Fibrogastroduadenoscopy can be performed routinely or urgently. An urgent examination is carried out to detect and remove a foreign body in the esophagus or stomach. The FGDS procedure is performed by an endoscopist using Japanese Pentax equipment.
How to prepare for research
Proper preparation of the patient for FGDS is one of the most important factors allowing for a full examination with minimal risk of “surprises”. Poor preparation makes gastroscopy difficult, reducing the information content of the procedure, or making it completely impossible.
Preparing the patient for the study, telling him in detail what’s what, convincing him to follow his recommendations is the direct responsibility of the doctor issuing a referral for gastroscopy. Measures to prepare for gastroscopy can be divided into general and local.
General preparation for FGDS includes the following measures:
- positive psychological attitude (most patients are terribly afraid of this study; the doctor must convince the patient of the need for it to be carried out for subsequent successful treatment; especially emotional and impressionable patients may be prescribed sedatives or tranquilizers a few days before gastroscopy);
- identification of conditions on which the choice of drugs for preparation for the procedure depends (pregnancy, lactation, allergic reactions to local anesthetics (lidocaine or others), glaucoma (atropine cannot be used) and others);
- if the patient has violations from the category of relative contraindications, their correction (prescription of antihypertensive, antiarrhythmic and other drugs).
Local preparation for FGDS:
- treatment of inflammatory diseases of the throat and esophagus (pharyngitis, tonsillitis and others) - the route of the gastroscope;
- diet (for 48 hours before gastroscopy, the patient is prohibited from consuming fried, difficult-to-digest foods that cause increased gas formation, or alcohol); the patient is prohibited from smoking for 2 hours before the study;
- cleansing the stomach of contents (the procedure must be carried out on an empty stomach; the patient is prohibited from eating the day before after 19:00; the presence of food in the stomach will not only make the study uninformative, but will also lead to an incident - gagging that occurs during the insertion of the gastroscope will provoke vomiting and pushing out the endoscope from vomit; this is not only unpleasant, but also very dangerous - the doctor simply does not have time to carefully remove the probe, which can cause damage to the stomach, esophagus or larynx);
- the use of additional symptomatic drugs (to speed up the process of digesting food, its exit from the stomach into the intestines, the patient may be recommended enzyme preparations - Mezim, Creon, Panzinorm; in case of increased gas formation - 5-10 minutes before the Espumizan test; in case of noticeable psycho-emotional overstrain by regarding the upcoming procedure - a sedative);
- the use of local anesthetics (in order for the patient to experience a minimum of discomfort during the insertion of the probe and the examination as a whole, his throat is treated with lidocaine or dicaine before the procedure);
- If the patient uses removable dentures, they must be removed immediately before the examination.