Causes
Enteritis is a group of diseases that are not age-related, so both children and the older generation are at risk.
The causes of the disease are classified according to form. The causative agents of the acute form are bacteria or viruses, excessive consumption of spicy and fatty foods, poisoning with toxic substances and alcohol, allergies to medications or certain types of products. The manifestation of enteritis in acute form can be caused by medical operations on the gastrointestinal tract and uncontrolled use of medications without a doctor’s prescription. The following factors contribute to the development of chronic enteritis:
- helminths;
- constant overeating;
- hereditary pathologies;
- congenital developmental anomalies;
- autoimmune diseases;
- lack of enzymes for digestion;
- untreated acute enteritis;
- abuse of heavy and rough foods;
- diseases of internal organs;
- injuries in the abdominal area.
Abuse of fast food, poor chewing of food, sedentary lifestyle and bad habits also provoke the development of the inflammatory process.
Reasons for the development of enteritis
Enteritis can be a consequence of acute intestinal infection, poisoning with toxic substances (for example, arsenic) or poisonous products (for example, mushrooms), abuse of fatty foods or alcohol, food or drug allergies, infection with helminths, etc.
Enteritis can also be caused by an enterovirus infection. Enterovirus infection can be called a relatively new disease, since enteroviruses (there are more than 60 types) began to be isolated only in the middle of the 20th century. Children under 10 years of age are most susceptible to enterovirus infection. The transmission of the virus is carried out both by airborne droplets, food, and household contact; the incubation period lasts from 1 to 10 days, so in a children's institution almost 2/3 of the team becomes infected with enterovirus infection. Characteristic symptoms of enterovirus infection are a sudden increase in body temperature to 38-40°, weakness, abdominal pain, flatulence, nausea and vomiting, loss of appetite, coating on the tongue, sore throat, etc. However, the disease can be asymptomatic. Unfortunately, enteroviruses can often cause various serious diseases in a patient, one of which is enteritis.
Also, enteritis is often associated with other diseases of the gastrointestinal tract and occurs after surgical interventions on the organs of the digestive system.
Among the factors contributing to the development of enteritis are smoking, atherosclerosis, renal failure, a tendency to allergies, autoimmune diseases, etc.
Symptoms of the disease
Each form of enteritis is accompanied by a specific clinical picture. But there are also general signs indicating the development of the disease. One of the main symptoms of enteritis is stool disorder with a strong urge to defecate immediately after eating. The picture is complemented by high blood pressure, hand tremors, and rapid pulse.
Other symptoms of enteritis include bloating and rumbling in the abdomen, the urge to vomit, and frequent abdominal pain, especially when eating. Appetite decreases, and along with it body weight, temperature rises, fatigue, tingling and coldness are felt in the extremities. External signs include: brittle nails and hair, dry skin, pallor. Puberty people notice a decrease in libido and menstrual irregularities.
Symptoms of acute enteritis:
- high body temperature (up to 39º);
- vomiting and diarrhea;
- persistent pain in the abdominal area;
- signs of dehydration: dry mouth, coated tongue, cramps.
The chronic form is characterized by the presence of the following symptoms: low blood pressure, problems with bowel movements, mild pain, and the development of anemia. If you notice one or more symptoms, you must immediately make an appointment with a specialist.
Enteritis chronic
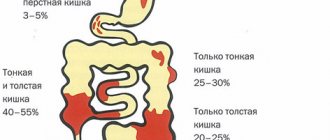
Chronic enteritis is an inflammatory-dystrophic pathology of the small intestine, leading to disruption of its digestive, transport and barrier functions. The symptoms include local (stool disorders, flatulence, abdominal pain) and general (increased fatigue, irritability, headaches and dizziness, problems with skin, nails and hair, endocrinopathies) signs, disorders of all types of metabolism. The diagnostic program includes stool analysis, coprogram, ultrasound of the obstructive tissue, x-ray and endoscopic examination with biopsy. Treatment is conservative and consists of prescribing a diet, antibacterial, replacement and symptomatic therapy. Chronic enteritis is a disease of the small intestine that develops as a result of degeneration or atrophy of the mucosa. Causes leading to chronic enteritis: infection (dysentery bacillus, staphylococci, salmonella, viruses), invasion by parasites (giardia, roundworm), exposure to industrial poisons (phosphorus, arsenic, lead), certain antibiotics (peomycin), salicylic group medications (aspirin) , allergic damage to the mucous membrane of the small intestine. Chronic enteritis can develop after gastrectomy, with chronic pancreatitis, hepatitis, liver cirrhosis, renal failure, various skin diseases (psoriasis, eczema)
Symptoms and course:
Pain of varying intensity in the middle parts of the abdomen, intensifying in the afternoon, sometimes cramping like “intestinal colic”, subsiding with the appearance of a loud rumbling. Abdominal bloating, feeling of fullness. During the period of exacerbation, diarrhea 3-6 times per knock, feces are abundant, light yellow in color, without admixture of blood, mucus or pus; in severe cases, the frequency of stools can reach 15 times a day. Possible disturbances such as dumping syndrome, hypoglycemic phenomena: voracious appetite, cold sweat 2-3 hours after eating.
With a long or severe course of chronic enteritis, symptoms of impaired absorption of substances necessary for the body are observed: weight loss, swelling, most often of the lower extremities, signs of hypovitaminosis, iron deficiency anemia, dystrophy of internal organs, including the liver, myocardium.
Recognition:
When examining blood, a decrease in the content of potassium, calcium, magnesium, iron, and protein is possible. Scatological examination of stool: undigested fats, fiber, large amounts of mucus and leukocytosis. Dysbacteriosis is detected. An X-ray examination determines the acceleration or deceleration of the passage of barium from the stomach through the small intestine, changes in the relief of its mucosa, and spasms of certain areas.
Treatment:
Treatment of chronic enteritis is carried out by a gastroenterologist. This pathology is characterized by a long and severe course with frequent periods of exacerbation, therefore all patients require a treatment regimen and a special diet. Food must be chemically, thermally and mechanically gentle and contain all necessary nutrients, vitamins and microelements.
Medications are prescribed to eradicate the infectious agent and normalize the intestinal microflora (eubiotics); astringent, enveloping and absorbent drugs; if necessary, gastric juice and pancreatic enzymes; means for normalizing intestinal motility, against diarrhea. Symptomatic treatment includes correction of metabolic disorders, vitamin therapy, hormone replacement therapy, and immunomodulators. For chronic enteritis, treatment with herbs and mineral waters, sanatorium-resort activities, and physiotherapy are indicated.
Diet, depending on the severity of the disease, eating 5-7 times a day with equal intervals between them, all food is warm and pureed. It is necessary to limit the amount of animal fats.
Vegetables and fruits are best pureed. Lean beef, veal, chicken, fish, eggs and cottage cheese, slimy soups, pureed porridge.
Avoid milk, brown bread, carbonated drinks, and for diarrhea - prunes, grapes, cabbage, nuts, freshly baked flour products. In a hospital setting, “fasting” days are carried out as prescribed by a doctor.
When dysbacteriosis is detected, the issue of prescribing appropriate medications is decided: sulfonamides, antibiotics or biological drugs (colibacterin, bificol, bifidum). If protein metabolism is disrupted, administer protein drugs. B vitamins, ascorbic acid injections. Against frequent heavy diarrhea - astringents. For anemia, iron supplements, vitamin B, and folic acid are indicated.
Diagnosis and treatment
For diagnosis, you need to collect anamnesis, clarify the symptoms and nature of the pain. But one survey is not enough, so diagnostic manipulations include several steps:
- Tapping the abdominal wall.
- General blood analysis.
- Coprogram.
- Bacteriological examination of stool.
- Ultrasound of the gastrointestinal tract.
Other diagnostic methods may be added to the listed studies.
Treatment of the disease takes place in two directions: elimination of primary symptoms and treatment of the causes that caused the disorder. The acute form of enteritis requires hospitalization and observation of the patient. If the form of the disease is viral, the patient is quarantined until complete recovery. In severe cases and the appearance of necrosis of internal organs, surgical intervention will be required.
As first aid for the treatment of enteritis, adsorbents are used: activated carbon, smecta, polysorb. Other treatment methods include taking enzyme preparations, antibiotics, probiotics, antihistamines, vitamin complexes and other medications appropriate to the type and form of the disease. The treatment regimen often includes taking antidiarrheals, antispasmodics, sedatives and antipyretics.
Folk remedies have also proven themselves to be effective in the treatment of enteritis. For example, rice water, dill seeds, chamomile, sage or St. John's wort infusions. However, they must be taken as prescribed by a doctor, as an auxiliary herbal medicine, and not as the main treatment.
Treatment
Diet therapy
In the treatment of patients with malabsorption syndrome (MS), a balanced diet plays an important role. The choice of dietary table depends on the underlying disease, but the diet must contain a sufficient amount of proteins (120-130 g per day), consumed in the form of dishes from lean meats, fish, cottage cheese, eggs. Easily digestible soy protein is shown. (The fat content should be 70-80 g per day due to the inclusion of easily digestible fats of plant origin in the diet. Animal fats should be used sparingly. The diet must contain foods rich in calcium (cottage cheese, cheeses) and potassium (raisins, bananas, dried apricots) .
Dairy products are prescribed as tolerated in the absence of direct contraindications (lactase deficiency). It is most advisable to include fermented milk products (kefir, yogurt, bifido products) in the diet.
In extremely severe cases of SM, accompanied by anorexia and exhaustion, it is necessary to resort to enteral tube feeding using special mixtures - enpits, etc.
Drug treatment
The main principles of treatment for SM are:
- improvement of cavity digestion;
- correction of dysbacteriosis;
- increasing the time of contact of chyme with the mucous membrane;
- reduction of intestinal secretion and stimulation of absorption;
- correction of metabolic disorders.
The main method of correcting impaired cavity digestion due to malabsorption is enzyme replacement therapy.
It is used to correct complete enteral syndrome in chronic pancreatitis, gastritis with secretory insufficiency, and other diseases. In this case, either a true deficiency of pancreatic enzymes occurs or a weakening of their activity. In the treatment of SM, it is preferable to use drugs with high enzymatic activity, for example Creon. Creon microspheres (1.2-1.7 mm in size) are enclosed in a gelatin capsule. Each microsphere has a protective coating that protects it from the destructive effects of hydrochloric acid and pepsins, which inactivate all previously existing enzyme agents. Creon will satisfy all the standard requirements for modern enzyme products: optimum action in the pH range from 4 to 7, high concentration of enzymes. One capsule of the drug contains 8,000 units of active lipase, while a festal tablet contains only 10 units. Creon is prescribed with food. The daily dose depends on the degree of SM and is 1-2 capsules 3-4 times a day. An even more active drug is paicitrate, containing 25,000 units of active lipase per capsule, which allows you to reduce the daily dose to 3-4 capsules per day. It is quite obvious that the use of conventional enzyme preparations (festal, panzinorm, mezim-forte, enzistal, etc.) to solve therapeutic problems would require taking 16-20 or more tablets per day, which is very undesirable for the patient.
The duration of taking enzyme agents depends on the cause of SM and on the speed of achieving a therapeutic effect. During therapy, it is usually not possible to limit oneself to a course of prescription and maintenance therapy is required (1-2 capsules of Creon per day), but if SM is not associated with pathology of the pancreas, and disorders of the cavity digestion are secondary (pathology of the liver, intestines, etc.), then enzyme preparations are used for symptomatic purposes, until the clinical and laboratory signs of SM, and most importantly, diarrhea, disappear.
One of the pathogenetically substantiated methods of treating SM is drug correction of dysbiosis. Restoring normal microbiocenosis of the gastrointestinal tract helps to normalize the processes of digestion and absorption of essential nutrients. Currently, the principles of treatment of dysbiosis have been radically revised, and what comes to the fore is not the desire to suppress the growth of opportunistic flora with antibacterial agents, but the restoration of the growth of saprophytic flora - bifidobacteria and lactobacilli, normal strains of E. coli, etc.
Normal microflora enters into an antagonistic relationship with pathogenic and opportunistic microflora, suppressing its growth and reproduction. One of the methods for restoring eubiosis is considered to be “functional nutrition”, which includes several groups of food components:
— dietary fiber (cellulose, hemicellulose, pectin, wheat bran — “Fibromed”);
- lactic acid mixtures;
- polyunsaturated fatty acids;
- aminosaccharides;
- antioxidants (vitamins E, C, beta-carotene).
In the treatment of dysbiosis, so-called “probiotics” (“eubiotics”) are widely used, which improve the microecological state of the body. All of them predominantly stimulate lactic acid and bifidobacteria.
Biological bacterial preparations containing live weakened strains of normal intestinal microflora include Lactobacterin, Bifidumbacterin, Bifical, Colibacterin, Bactisubtil, Linex, Bifiform, etc. Of the probiotics made on the basis of microbial metabolites, the most effective is Hilak-Forte. The use of new probiotics based on Bacillus subtillis, containing spores of these bacteria and their recombinant agent, subalin, is promising. The latter is prescribed 1-2 doses 3-4 times a day for 10-14 days. Enterol (medicinal yeast), which is a lyophilized culture of the fungus Saccharumyces Boulardi (Saccharomyces boulardi), has a similar effect, which has high antagonistic activity against clostridia, Shigella, Escherichia, etc. Recently, laminolact, a complex drug, has been used for the treatment of dysbiosis. containing live, non-lyophilized cultures of some bacteria, protein hydrolysate, fruit pectin, seaweed. It is advisable to use it in the form of tablets or capsules (3 tablets 3 times a day for 3 weeks).
Antibacterial therapy for dysbiosis should be carried out only in cases of persistent diarrhea caused by high activity of opportunistic microbes or with obvious symptoms of inflammation, accompanied by fever, arthralgia, and general intoxication. In this case, you should resort to intetrix, nitroxaline, 5-NOK, enterosediva, etc. Treatment is carried out in short courses (5-7 days) in accordance with the sensitivity of the cultured pathogen. It is better to use hydroxyquinoline derivatives, broad-spectrum antiseptics that are not absorbed in the intestines and do not affect lacto- and bifid flora.
If anaerobic microflora (clostridium) is detected, treatment with metronidazole (tinidazole) is indicated. Nitrofuran drugs (furodonin, furagin, ercefuril) and nalidixic acid derivatives (navigramon, negram) are active against Proteus, enteropathogenic Escherichia, and Klebsiella. In any case, after antibacterial therapy, treatment with biological products to restore the microflora is indicated.
Motility inhibitors are used as one of the treatment methods for SM. These drugs reduce the peristaltic activity of the small intestine and increase the time of contact of chyme with the mucous membrane, which improves absorption. For this purpose, Imodium (loperimide) is used, which actively inhibits the motor activity of the small intestine and relieves diarrhea. The dose of the drug must be selected individually.
Astringents and sorbents have a certain symptomatic effect in SM. The purpose of their purpose is to bind excess fluid, toxins and bacterial agents in the intestinal lumen. The most active in this regard is smecta, which is a cytomucoprotector and a selective sorbent at the same time. The drug has a distinct antidiarrheal effect, reduces the loss of fluid and electrolytes, restores the integrity of the mucous barrier and the glycocalyx of enterocytes. (Smecta has a beneficial effect on the content of normal intestinal microflora and does not absorb food ingredients, vitamins and enzymes. To improve the absorption of water and electrolytes, sometimes, especially in old age, the administration of short courses of glucocorticoids (prednisolone) is justified. This activates Na + K +-ATPase in enterocytes, the general condition and well-being of patients improves. An important component of the treatment of SM is the correction of all types of metabolic disorders. Treatment is purely symptomatic and is carried out according to indications. To restore protein deficiency, intravenous administration of amino acid mixtures (aminocrovin, alvesin and etc.) and native proteins homologous to plasma proteins (albumin, native or frozen plasma, protein). For better absorption of proteins, it is necessary to simultaneously prescribe anabolic steroids (Nerobol, Nerobolil, Retabolil). To correct fat metabolism, fat emulsions (lipofundin, etc.) are administered intramuscularly .).
In cases where active rehydration and restoration of electrolyte shifts are necessary, patients are given intravenous drips of hamodez, rheopolyglucin, electrolyte solutions (potassium chloride, calcium chloride or gluconate, disol, etc.).
For the treatment and prevention of osteoporosis, the use of the active form of vitamin D (D3), which enhances calcium absorption, is indicated. In case of anemia development, treatment is carried out with iron supplements, vitamin B12 and folic acid, taking into account the genesis of anemia.
Celiac disease and Whipple's syndrome, which include SM, but have a number of specific features in terms of etiology and pathogenesis, as well as clinical presentation and treatment, are subject to separate consideration.
Diet table
When treating enteritis, it is necessary to adhere to the correct drinking and nutrition regimen. Drinking small portions of water every 10–15 minutes will help avoid dehydration. You need to drink simple purified water, avoiding sugary carbonated drinks, milk, alcohol, coffee and juices. It is important to exclude from the diet:
- roast;
- fresh fruits and vegetables;
- legumes;
- smoked;
- strong broths;
- semi-finished products.
Try to eat steamed or baked foods without fat or salt. For example, potatoes, fish, and meat have proven themselves well. It is recommended to enrich the diet with low-fat cottage cheese, fermented milk products, jelly, and oatmeal. Prepared food should be thoroughly chopped or pureed and taken in small portions five times a day.
Prevention and prognosis
The disease is not particularly dangerous, but enteritis that is not treated in time can be fatal. Mild to moderate treatment safely returns the patient to normal life within a few days. An advanced degree of enteritis provokes chronic inflammation and atrophy of the small intestine. The inability to digest food leads to death. Other complications include heart failure, kidney and liver disease, and intestinal perforation.
Following simple rules will help you avoid the appearance of enteritis:
- Balanced diet.
- Careful processing of products.
- Compliance with personal hygiene rules.
- Take medications only as prescribed by a doctor.
- Timely consultation with specialists to identify hidden diseases and pathologies.