Gastritis of the stomach: symptoms, treatment regimen and nutritional rules
Gastritis is a common disease that involves inflammation of the gastric mucosa due to the influence of factors of various origins, gradually leading to dystrophic changes in the epithelium.
Morphological changes that progress over time cause disruption of the functioning of the organ, which affects the patient’s well-being and worsens his quality of life.
Depending on the degree of damage and the duration of exposure to irritating factors, acute and chronic forms are distinguished.
Reasons for development
Symptoms of the disease occur when the gastric mucosa is damaged. Various factors influence:
- irregular eating, undereating and overeating, rushing while eating;
- poor chewing of food, often associated with poor dental health;
- low-quality products, abuse of fried, hot, spicy, rough foods;
- insufficient intake of protein and vitamins, which causes less gastric juice to be produced;
- regular drinking, smoking;
- long-term use of medications: antibiotics, aspirin, hormonal drugs;
- ill health of the digestive system, impaired peristalsis, causing bile to end up in the stomach and cause inflammation of the mucous membrane;
- signs of gastritis appear in case of imbalance of intestinal microflora, penetration of viruses, bacteria, streptococci, staphylococci, salmonella.
Chronic gastritis in adults occurs with poor quality or incomplete treatment of the acute form. Intestinal infections, inflammation of the tonsils or gallbladder, infection with Helicobacter pylori maintain the chronic form. It develops in hazardous production conditions, when dust, fumes of acids or alkalis, and harmful chemical compounds are ingested every day. Constant inflammation of the gastric mucosa is associated with one or another allergy.
The gastric juice contains pepsin to break down protein foods. If a malfunction occurs, pepsin acts on the mucous membrane containing protein, causing inflammation as the stomach begins to digest itself.
Causes of the disease
The most common cause of gastritis is infection with the bacteria Helicobacter pylori. These are one of the few microorganisms that can survive in the aggressive environment of gastric juice. Other causes of the disease usually include:
- The effect of chemical irritants (in particular, alcohol and some medications with prolonged use).
- Chronic stress.
- Parasitic infections.
- Autoimmune processes are damage to mucosal cells by cells of the immune system.
- Reflux of bile acids into the stomach (reflux gastritis).
- Identification of the etiological factor is important, since the treatment tactics of the disease depend on it.
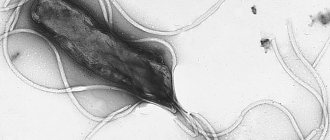
The role of Helicobacter pylori in the development of gastritis
In the second half of the 20th century, a previously unknown factor was identified, which today is considered one of the first places in the etiology of chronic gastritis. Helicobacter pylori is a spiral-shaped gram-negative bacterium that infects various areas of the stomach and duodenum.
Many cases of gastric and duodenal ulcers, gastritis, duodenitis, and possibly some cases of gastric lymphoma and gastric cancer are etiologically associated with Helicobacter pylori infection. The successful experience with self-infection of one of the discoverers of the role of Helicobacter pylori in the development of diseases of the stomach and duodenum, Barry Marshall, and a group of volunteers served as convincing evidence of this theory. In 2005, Barry Marshall and his colleague Robin Warren were awarded the Nobel Prize in Medicine for their discovery.
However, the majority (up to 90%) of infected Helicobacter pylori carriers do not show any symptoms of disease. Not every chronic gastritis has a bacterial cause.
Classification
There are several types of acute gastritis:
| Simple (catarrhal) gastritis | develops as a result of ingestion of stale food contaminated with pathogenic microbes (foodborne toxic infection), with rotavirosis, an allergy to some food product, or as a result of damage to the gastric mucosa by certain medications. With catarrhal gastritis, the mucous membrane is destroyed slightly (only the most superficial layer) and is quickly restored after the irritating factor ceases. |
| Erosive gastritis | develops after some concentrated acids or alkalis enter the stomach (chemical burn of the gastric mucosa). With corrosive gastritis, not only the superficial, but also the deep layers of the gastric mucosa are destroyed, so this form of the disease often gives rise to peptic ulcers or scar formation. |
| Phlegmonous gastritis | This is a purulent inflammation of the stomach, which can develop as a result of a foreign object (for example, a fish bone) entering the stomach wall, followed by infection of this area with a pyogenic infection. A distinctive feature of this type of gastritis is high fever and unbearable pain in the epigastric region. Phlegmonous gastritis requires immediate surgical intervention. Without medical assistance, the disease progresses to peritonitis (extensive inflammation of the abdominal organs) and ends in death. |
| Fibrinous gastritis | occurs very rarely against the background of sepsis (blood poisoning). |
Gastritis has many varieties. A brief description of each type can be found below:
| Low acidity | insufficient concentration of acid in gastric secretions, which creates conditions for weak fermentation of incoming food. As a result, the walls of the stomach can be damaged by rough pieces of food, and the body does not receive the required amount of substances. |
| With high acidity | increased concentration of gastric juice, forming persistent, sometimes causeless heartburn. The atypical saturation of the enzyme fluid stimulates the formation of multiple ulcerations on the mucosa. |
| Atrophic | gradually leads to thinning of the epithelium of the stomach, degeneration of the glands into simpler forms and a decrease in the quality of the work they perform. Without corrective therapy, it can cause cancer. |
| Antral | develops against the background of infection by Helicobacter pylori culture, leading to focal modifications of the internal epithelium. The result of bacterial activity is scarring of the mucous membrane and insufficient formation of gastric secretions. |
In professional medicine, other classifications of gastritis are also used, including according to the type of distribution of pathogenesis:
- Autoimmune gastritis (type A);
- Exogenous gastritis (type B), provoked by Helicobacter pylori;
- Mixed gastritis (type A+B);
- Gastritis (type C), provoked by NSAIDs, chemical irritants or bile;
- Special forms of gastritis;
- Gastritis against the background of decreased and increased secretion of hydrochloric acid;
- Other forms of morphological and functional manifestations of gastritis.
Their differentiation involves the use of complex medical laboratory or instrumental techniques at the stage of diagnosing the disease. Therefore, a description of gastritis, which has approximately the same clinical symptoms, but differs in the underlying mechanisms of pathogenesis, is not of interest to a wide range of readers.
Let us dwell in detail on the main signs and symptoms of gastritis, which may serve as the basis for a person to contact a medical institution for help.
How to treat gastritis
Treatment is selected depending on the type of disease, concomitant pathologies, the patient’s age and a number of other features. The basis of treatment for almost all types of gastritis is diet in combination with pharmacotherapy. Medicines are selected depending on the level of stomach acidity and the etiological factor.
Features of treatment of different types of gastritis
There is much in common in the treatment of gastritis, but each type has its own nuances. In this regard, independent treatment is unacceptable. The doctor selects an individual treatment regimen depending on a number of factors. Let us consider in more detail the features of treatment of various types of disease.
Surface
Treatment of superficial forms of gastritis includes mandatory diet therapy and drug treatment. Depending on the etiological factor and a number of other features, drug therapy may include taking antibiotics to eradicate Helicobacter pylori, as well as drugs that regulate acidity levels. Some patients are also prescribed coating drugs and gastroprotectors.
Chronic superficial
Treatment of the chronic form of superficial gastritis largely depends on the secretory function of the stomach. If we are talking about low acidity (which is most often observed in elderly patients), then treatment table No. 2 is prescribed. The patient is prescribed drugs based on digestive enzymes, gastric juice, as well as drugs that stimulate the production of hydrochloric acid by the parietal cells of the mucosa.
In case of increased acidity, medications that normalize the acidity level are indicated. Drugs that have an enveloping and antispasmodic effect are also prescribed. If the bacterial nature of chronic superficial gastritis is established, then antibiotics are prescribed.
Chronic atrophic
Treatment of atrophic forms of pathology depends on the root cause of the disease. It is important to establish the pathogenesis of atrophic gastritis: association with Helicobacter pylori or autoimmune processes.
As with other types of gastritis, with the atrophic form, the basis of treatment is diet therapy and drug treatment. If the disease is associated with prolonged infection by Helicobacter pylori, then antibiotic therapy is carried out.
Unfortunately, with the autoimmune form of atrophic gastritis, everything is much more complicated. Currently, it is almost impossible to eliminate the autoimmune component of the disease. Glucocorticoids are usually used to suppress the activity of the immune system, but their use is only advisable in cases where the disease is accompanied by pernicious anemia (caused by a lack of vitamin B-12). In other cases, the side effects of glucocorticoids will prevail over the possible therapeutic effect.
Erosive
Most often, treatment of erosive gastritis is conservative. As in other cases, the patient is required to strictly adhere to the diet and take medications as prescribed by the doctor. In the vast majority of cases, these measures are sufficient to achieve the desired therapeutic effect.
In rare cases, with an erosive form of pathology, endoscopic hemostasis is resorted to - a surgical operation aimed at stopping gastric bleeding. In very rare cases, a patient with an erosive form of gastritis is indicated for gastrectomy - removal of the stomach.
Chronic anacid
As with the atrophic form, anacid gastritis can have both bacterial and autoimmune etiologies. Drug therapy is selected depending on the etiological factor. When it comes to Helicobacter pylori infection, amoxicillin and clarithromycin are most often used. In some cases, tetracycline antibiotics and bismuth preparations are also used to eradicate Helicobacter pylori.
As for autoimmune gastritis, treatment is symptomatic. The patient is prescribed antispasmodic and painkillers, as well as medications that stimulate gastric motility. In this case, diet remains a fundamental element of therapy.
Diet therapy
Source: lsantilli / Depositphotos
The most important condition for the successful treatment of all forms of gastritis is diet. Let's consider the fundamental rules of nutrition for this disease:
- Chew your food thoroughly. Poorly chewed food irritates the gastric mucosa, thereby aggravating the course of the disease.
- Fractional meals. If you have gastritis, you need to eat often - 5-6 times a day in small portions. At the same time, it is important to monitor your daily caloric intake so that there is no excess.
- Follow your diet. Try to eat at the same time every day. This way the body will get used to a certain regime and will know when to prepare for meals.
Diet for different forms of gastritis has much in common. For example, in almost all forms of the disease, you should not eat a lot of sour fruits and vegetables. Plant foods should only be eaten stewed, boiled or baked. You can learn more about the intricacies of diet for different types of gastritis in our material “Diet for Gastritis.”
Medicines for gastritis
Various types of drugs are used to treat gastritis. Depending on the cause of the disease, the patient is prescribed medications that regulate acidity levels, antibiotics, antispasmodics and painkillers. Let's take a closer look at these groups of drugs:
- Antacids are drugs that have a neutralizing effect on hydrochloric acid. It is advisable to use antacids for gastritis with high acidity.
- Alginates are preparations with an enveloping effect. Thanks to this effect, it is possible to reduce the aggressive effect of gastric juice on the mucous membrane. Accordingly, alginates are also used for increased stomach acidity.
- Antispasmodics are drugs that eliminate spasms. The action of these drugs is aimed at relaxing the muscles. As a rule, drugs based on drotaverine or papaverine are used among antispasmodics.
- Analgesics are painkillers used for pain of various origins.
- Antibacterial drugs - used for proven bacterial origin of gastritis caused by Helicobacter pylori. Among antibiotics, amoxicillin is often used, and tetracycline antibiotics are less commonly used. Bismuth preparations, which are used in the treatment of gastritis of infectious origin, also have anti-Helicobacter activity.
- Gastroprotectors are drugs that protect the gastric mucosa. In this case, preference is given to bismuth preparations; they perform a dual function - they protect the mucous membrane and destroy Helicobacter pylori.
- Antisecretory drugs are drugs that reduce the production of hydrochloric acid by glandular cells of the gastric mucosa. Currently, proton pump inhibitors are most often used as antisecretory drugs.
- Prokinetics are drugs that improve the motility of the gastrointestinal tract. As a rule, prokinetics are used for gastritis with low acidity. Thanks to these drugs, the patient can avoid symptoms such as nausea and vomiting.
ethnoscience
Figure 3: Avocados won't cure gastritis, but they may be a healthier choice among nutritious sources of fat.
Source: Dream79 / Depositphotos Information about traditional methods of treating diseases of the gastrointestinal tract has survived to this day. At a time when there were no modern methods of diagnosing and treating gastritis, the disease was fought with various folk remedies. Among these the following can be noted:
- oat decoction;
- aloe juice;
- sea buckthorn oil;
- propolis;
- plantain infusion;
- potato and cabbage juices.
We remind you that traditional methods can only be used as an addition to the main treatment, and only with the permission of a doctor. Self-medication in this case is unacceptable, since folk remedies are ineffective.
Symptoms of gastritis in adults
The characteristic symptoms of gastritis in adults depend on the form of the disease. Acute gastritis is characterized by the following symptoms:
- nausea is constant or intermittent, often occurring immediately after eating;
- abdominal pain: sharp paroxysmal or constant painful. Often depends on food intake: worsens on an empty stomach or some time after eating;
- repeated vomiting, first of stomach contents with a sour smell and taste, then of clear mucus, sometimes greenish or yellow and bitter in taste (bile);
- heartburn - an unpleasant burning sensation in the chest that occurs after eating;
- belching with a sour smell, after eating or on an empty stomach;
- bowel dysfunction: constipation or diarrhea;
- increased salivation is the body’s reaction to indigestion; sometimes dry mouth (after several bouts of vomiting due to dehydration)
- from the whole body: severe general weakness, dizziness, headache, sweating, increased temperature, decreased blood pressure, increased heart rate - tachycardia.
High and low acidity
The most common signs of gastritis with low or zero acidity:
- constant unpleasant taste in the mouth;
- heaviness in the stomach after eating;
- burping “rotten eggs”;
- rumbling;
- nausea in the morning;
- problems with regularity of bowel movements;
- disgusting breath.
The most common signs of gastritis with high acidity, in addition to general symptoms (vomiting, nausea):
- prolonged pain in the solar plexus, disappearing after eating;
- frequent diarrhea;
- heartburn after eating sour foods;
- frequent urge to pass gas from the mouth - belching.
Types of gastritis
Hypoacid - this form of the disease causes a gradual decrease in the secretion of hydrochloric acid, and as a result, the stomach cavity completely atrophies. Because of this, food and all the beneficial microelements it contains are not absorbed. In addition, this type of gastritis is very dangerous due to the high likelihood of cancer.
The symptoms of such gastritis depend entirely on the degree of damage to the stomach. In the very initial stages of the disease, the patient may feel heaviness in the stomach, periodic pain after eating, or experience a feeling of nausea. The list of symptoms can also include belching, constipation, bloating and occasional vomiting.
The consequences of this type of gastritis are very unpleasant:
- deterioration of the skin, nails and hair;
- unhealthy weight loss;
- severe weakness and fatigue;
- dysbacteriosis in the oral cavity.
Diffuse - in this case, the entire mucous surface of the stomach becomes inflamed evenly. If the disease is not cured, it leads to gastric atrophy and the inability of the organ to digest food. Like hypoacid gastritis, this type of gastritis is dangerous because its advanced form leads to the development of oncology. Also among the consequences are:
- avitaminosis;
- general intoxication;
- weakness.
It is worth noting that several factors lead to the development of this gastritis. For example, this could be poor nutrition, fasting, alcohol abuse, smoking or severe viral diseases. In addition, the occurrence of the disease can provoke severe stress.
Antral - this inflammation is characteristic of the antrum. It does not go away without a trace and causes atrophy, which can remain with the patient forever. In a conversation with our publication, medical gastroenterologist and candidate of medical sciences Boldyreva Larisa Ivanovna said that the causative agent of this type of gastritis is the bacterium Helicobacter pylori. According to the doctor, this harmful microorganism enters the stomach in infancy, after which it continues to develop there. The bacterium is capable of secreting enzymes that cause irritation of the mucous membrane and provoke the constant release of hydrochloric acid. Because of this, the gastric glands suffer greatly. They literally die and are replaced by scar tissue.
At first, patients do not notice the symptoms and blame it on malnutrition and stress. However, over time, the disease develops and the condition of patients worsens. Its symptoms include:
- heartburn;
- burping;
- flatulence;
- bad breath;
- constipation;
- bloating.
Symptoms and their intensity depend entirely on food intake and lifestyle. This type of gastritis often leads to the development of cancer.
pixabay.com/valelopardo
Anacidic - this form is characterized by low acidity. In the presence of this disease, gastric juice is practically not produced, which means that undigested products remain inside the organ, which gradually poison the body. If the disease is neglected, there is a high risk of developing cancerous tumors.
This type of gastritis occurs more often in those people who lead a sedentary lifestyle. Characteristic features are:
- sour breath;
- increased pain after eating;
- constant feeling of heaviness in the stomach;
- general weakness.
Superficial - this form can be called one of the safest. However, if it is not treated and left untreated, the inflammatory process spreads to the duodenum, resulting in antral gastritis.
Most often, patients complain of pain in the solar plexus area. It occurs after eating spicy, very salty or sour foods, which cause severe irritation of the stomach cavity.
Erosive - this form is accompanied not only by an inflammatory process, but also by the occurrence of erosions on the inner surface of the stomach. The damage worsens over time, increasing the likelihood of internal bleeding.
It is worth noting that this form of gastritis is also caused by the aforementioned bacterium Helicobacter pylori. Very often, patients do not notice all the symptoms and decide to postpone treatment, but during the interview, Dr. Boldyreva advised not to joke about such things.
Important
“If this disease was caused by Helicobacter pylori, then treatment, of course, is carried out both during the period of remission and during the period of exacerbation. Most often, with gastritis caused by Helicobacter pylori, there are manifestations of an ulcer-like nature. Patients with an exacerbation caused by this form of gastritis often complain of pain that occurs either one and a half to two hours after eating, or on an empty stomach. Sometimes it manifests asymptomatically.”
Erosive gastritis is characterized by:
- constant aching pain;
- frequent heartburn;
- feeling of fullness in the stomach after eating;
- problems with stool.
Reflux gastritis is a condition caused by the constant entry of acidic contents into the stomach, due to which the mucous surface of the organ is severely damaged and gradually destroyed. Everything happens due to a malfunction of the pylorus, which provokes the return of almost digested food from the duodenum. At this point, food already contains a large amount of bile and various enzymes that have a detrimental effect on the organ.
Hyperplastic - this form of the disease provokes the proliferation of cells on the surface of the stomach. As a result, benign tumors and polyps are formed, which interfere with digestion and the absorption of beneficial enzymes. Over time, these neoplasms can become malignant.
A characteristic symptom is constant aching pain. As the disease progresses, the symptoms only intensify, causing:
- frequent vomiting;
- flatulence;
- feeling of heaviness.
Gastritis with high acidity - this form of the disease is characterized by a strong secretion of gastric juice, which literally eats away the walls of the stomach, leading to severe inflammation and destruction of the organ. It is characterized by severe heartburn after eating any food.
It occurs for various reasons. This may be due to excessive drinking, smoking, spicy foods or the presence of the Helicobacter pylori bacteria.
Gastritis with low acidity - in this case, the stomach loses its ability to normally process and absorb food due to decreased acidity. This leads to the fact that the bacteria contained in the food are not neutralized by the acid, but continue their life in the stomach, causing pain, bloating and belching.
Signs of exacerbation
Relapse of chronic gastritis is characterized by a variety of symptoms, the most common are the following symptoms:
- Increased salivation, thirst, weakness;
- Manifestations of dyspepsia (constipation, diarrhea);
- Dizziness, palpitations, headache;
- Nausea, morning vomiting of semi-digested food with a characteristic sour taste, sometimes vomiting bile;
- Constant or periodic pain in the solar plexus, which intensifies immediately after eating, or vice versa, with prolonged fasting;
- Belching with air, burning in the sternum, heartburn after eating, metallic taste in the mouth.
Symptoms of exacerbation of erosive (severe) forms of gastritis are supplemented by vomiting with blood clots, sometimes vomiting with dark-colored vomit. Gastric bleeding during bowel movements is manifested by black stool. Sometimes gastric bleeding can only be determined by laboratory methods. Massive internal bleeding is manifested by pallor of the skin and mucous membranes and is easily determined by the color of the sclera of the eyes, dizziness, and tinnitus.
Complications
Gastritis in adults (with the exception of phlegmonous gastritis) does not belong to the group of dangerous diseases. However, gastritis gives rise to dangerous complications:
- Stomach bleeding
- Peptic ulcer of the stomach and duodenum,
- Stomach cancer.
The effect of gastritis on the body as a whole is explained by a disorder of the digestive process. Patients with gastritis begin to “fear food”, lose weight, some vomit most of the food they eat, or suffer from heartburn after eating. Against the background of gastritis, vitamin deficiency and anemia often develop.
Diagnostics
Stages of diagnosing chronic gastritis:
- Endoscopic diagnosis with mandatory biopsy - the presence of Helicobacter pylori, the nature and localization of changes in the gastric mucosa, the presence of precancerous changes in the gastric mucosa are clarified. For a biopsy, at least 5 fragments are taken (2 from the antrum, 2 from the body of the stomach, 1 from the angle of the stomach).
- Clinical diagnosis - the patient’s complaints, anamnesis, examination data of the patient are analyzed, a presumptive diagnosis is made and a rational plan for instrumental examination is drawn up.
- Laboratory diagnostics - clinical blood test, biochemical blood test, clinical urine test, clinical stool test, stool occult blood test, detection of Helicobacter pylori infection.
- Respiratory diagnostics - the presence of Helicobacter pylori is specified. This method involves the patient taking urea of normal isotopic composition and then measuring the ammonia concentration using a gas analyzer.
- Intragastric pH-metry - determination of the state of secretion and diagnosis of functional disorders in acid-related gastrointestinal diseases.
- Ultrasound examination of the liver, pancreas, gall bladder - to identify concomitant diseases of the gastrointestinal tract.
- Manometry of the upper gastrointestinal tract, with the help of which the presence or absence of reflux gastritis is determined (normally in the duodenum the pressure is 80-130 mm water column, in patients with reflux gastritis it is increased to 200-240 mm water column .).
- Electrogastroenterography is a study of the motor-evacuation function of the gastrointestinal tract in order to determine duodenogastric reflux.
Establishing a clinical diagnosis is based on determining the type of chronic gastritis, assessing the prevalence of morphological signs of the disease, the presence and severity of gastric dysfunction.
Classification of drugs for gastritis: the most effective drugs
The table shows the most popular and effective drugs for the treatment of gastritis, which can be part of complex therapy. All data is for informational purposes and should not be used as a call for self-medication. Any prescriptions should be made only by the attending physician! Before starting to take medications, you should also consult a specialist, as there may be contraindications.
| Group of drugs | What drugs are included | Approximate cost (in rubles) |
| Proton pump blockers | "Omeprazole" | 80 |
| "Omez" | 400 | |
| "Zolispan" | 220 | |
| "Peptazol" | 220-230 | |
| "Rabelok" | 315 | |
| Ursodeoxycholic acid | "Ursolit" | 1250 |
| "Ursodez" | 1450 | |
| "Henofalk" | 970 | |
| Antihistamines | "Tavegil" | 310 |
| "Loratadine" | 40 | |
| "Claritin" | 350 | |
| "Suprastin" | 210 | |
| Means for protecting mucous membranes | "Biogastron" | 300 |
| "Venter" | 600 |
Treatment of gastritis can sometimes take from several months to several years. The main therapy is a therapeutic diet, but if it does not give the desired effect, the patient must be prescribed medications. It is highly undesirable to select them yourself, as there is a high risk of serious side effects. It is best to consult your doctor and undergo an examination to make an accurate diagnosis and prescribe competent treatment.
Treatment of chronic gastritis
In 90% of cases, chronic gastritis in adults is caused by the bacterium Helicobacter pylori. Therefore, with this disease, the first step is to examine the patient for the presence of this pathogen in the body. Also equally important is the analysis of gastric juice, which will help choose the optimal treatment.
The main stages of treatment of chronic gastritis in adults are as follows:
- Anti-Helicobacter therapy is carried out. It is performed for 10 days according to a 3-component scheme: hydrogen pump blocker, amoxicillin, clarithromycin. If it was not possible to achieve an effect, then after a month and a half the treatment is repeated according to a 4-component scheme. At the same time, de-nol is added to these agents.
- An appropriate diet is selected.
- Low acidity requires enzyme replacement therapy. For this purpose, multienzyme drugs are prescribed - enzistal, festal, mezim, abomin.
- If acidity is high, medications are used to reduce it. This reduces pain and heartburn and speeds up the healing process.
- The use of traditional medicine is permitted in combination with medications.
Modern approaches to the treatment of chronic gastritis have reduced the prevalence of this disease and significantly reduced the frequency of exacerbations. But despite this, Helicobacter infection can easily recur. Therefore, for those who want to forget about the disease for a long time, it is necessary to take care of eliminating predisposing factors.
Antispasmodics for gastritis
To reduce the severity of pain caused by spasm of the muscles of the gastric walls, you can use antispasmodics. Most often, patients are prescribed the following drugs of this pharmacological group:
- "No-shpa";
- "Drotaverine";
- "Papaverine".
Children can use Papaverine in the form of rectal suppositories. They need to be inserted after defecation. To avoid leakage of the suppository, you must remain in bed for at least 30 minutes after using the medicine, so it is best to use them at night.
Treatment of acute gastritis in adults
Acute gastritis resulting from ingestion of concentrated chemicals is often accompanied by laryngeal edema and renal failure, requiring emergency medical intervention. Therefore, such conditions cannot be treated at home. The main therapeutic measures carried out for acute gastritis are as follows:
- Gastric lavage. For this purpose, the patient is asked to drink several glasses of water or saline, and then, by pressing on the root of the tongue, they induce vomiting. This procedure is repeated until the vomit contains food particles.
- Complete fasting during the first day, taking only weak tea, rosehip, chamomile or mint decoction. You can also drink still mineral water.
- After this, prescribe a gentle diet - pureed mucous soups, omelettes, soufflés made from lean meats or fish, jelly.
- To relieve nausea and vomiting, Motilium or Cerucal is recommended for this purpose.
- Relieving pain and eliminating spasms with platyphylline and papaverine.
- For severe toxic infections, prescribe antibacterial therapy.
Gastritis of allergic origin requires keeping a food diary and following an elimination diet.
Folk remedies for gastritis
It is very important to take into account whether the acidity of the stomach is high or low.
- If you are worried about constipation in the anacid form of gastritis, you need to take laxatives based on buckthorn bark and rhubarb.
- If the acidity is high, it is tedious to drink 100 ml of potato juice up to three times before meals every day.
- In autumn, gastritis can often worsen; in this case, you need to brew fresh blueberries and strawberries, consume 100 ml before meals.
- In cases of problems with appetite due to illness, herbalists recommend bitterness - decoctions based on dandelion, wormwood, and yarrow. It is good to add soothing herbs - valerian, motherwort and those that stimulate the stomach - licorice, calendula, plantain.
- If you have low acidity, you are advised to pay attention to this collection; it contains dandelion, calamus root, chamomile, calendula, St. John's wort, and plantain.
- For high acidity, this collection is recommended; it will require linden blossom, peppermint, calamus root, licorice, fennel, and flaxseeds.
Thus, gastritis must be treated at the initial stage so that it does not develop into an ulcer or cancer over time.
Diet for gastritis, what can and cannot be eaten?
Nutrition for gastritis depends on the form and course of the disease. In case of acute gastritis and exacerbation of chronic gastritis, a strict diet is indicated; in the remission phase of chronic gastritis, the diet can be expanded. For any type of gastritis, alcohol, smoking, fried, fatty, and spicy foods are strictly excluded. You should also never go hungry.
What you can and cannot eat depends on the type of gastritis: if the acidity of the stomach is increased, it must be reduced, and if gastritis occurs with atrophy of the mucous membrane, it is necessary to stimulate the functioning of the remaining glands.
Forecasts
The prognosis for the treatment of gastritis in adults largely depends on the patient himself - his or her discipline. Unfortunately, many people neglect their diet, thereby causing complications and exacerbations.
The question of complete recovery from gastritis also depends on etiological factors. As mentioned above, bacterial forms of pathology can be treated with antibiotics. If we are talking about gastritis of an autoimmune nature, then the disease is incurable, and in this case only symptomatic treatment is possible.
Important : acute and chronic gastritis. Acute forms of gastritis are much easier to treat. Therefore, at the first acute symptoms, consult a doctor immediately. Do not allow the disease to become chronic.
Nutrition for low stomach acidity
For gastritis with low acidity and atrophic gastritis, an important point in the diet is the stimulation of gastric secretion. Meals should be taken at certain hours (a strict eating schedule normalizes the process of secretion of gastric juice). Food should evoke a feeling of appetite, it should be taken in a calm environment, without haste. It is important to chew food thoroughly: on the one hand, crushed food will not injure the gastric mucosa, on the other hand, while we chew, a large amount of gastric juice and saliva are produced, which contribute to the best absorption of food.
For gastritis with low acidity, you should exclude:
- salty, spicy dishes;
- mushrooms, coarse stringy meat;
- alcohol;
- foods fried in oil, baked dishes;
- cabbage, grapes and grape juice.
What can you eat if you have gastritis with low acidity:
- fish fillet from low-fat fish;
- meat: rabbit, chicken in the form of boiled meat, low-fat cutlets, meatballs; meat broths, fish soup;
- sour cream, kefir, cottage cheese, milk, cheese;
- vegetable purees, grated vegetable salads from potatoes, beets, carrots, zucchini, spinach;
- mineral water 20-30 minutes before eating.
- fruit juices (except grape), compotes, decoctions of rose hips, black currants;
Meals are taken at least 5 times a day. Therapeutic nutrition is followed for another 2-3 months after the exacerbation. The patient should be in a calm environment, with conditions for good rest and sleep. It is recommended to take vitamin and mineral supplements.
How to choose the right nutrition
For each form of gastritis, a separate diet is prescribed, which the patient must follow for the entire period of treatment. But it is still possible to highlight individual foods and dishes that are allowed to be eaten with gastritis. Among them:
- broths from lean meat and fish,
- dietary meat;
- steamed casseroles and cutlets;
- baked and boiled vegetables without seasoning;
- porridge cooked in water;
- boiled chicken eggs.
Some patients are prescribed baby food during an exacerbation. However, we advise you to consult a doctor and not select diets on your own.
Nutrition for high stomach acidity
When following a diet for gastritis with high acidity, it is recommended to exclude:
- Products that stimulate the production of gastric juice: alcohol, carbonated drinks, grape juice, coffee, cabbage, rye bread, legumes, sausages, smoked fish
- Products that damage the already inflamed gastric mucosa: mushrooms, fatty meat (lamb, pork, duck), radishes, wholemeal bread.
- Eating very hot or cold food: hot food damages the gastric mucosa, cold food stays in the stomach longer and causes an increase in the production of hydrochloric acid.
- Food fried in oil; fatty foods, fresh baked goods.
- Limit seasonings as much as possible: salt, pepper, garlic, mustard.
What can you eat with this type of gastritis:
- Low-fat boiled meats: chicken, pigeon, rabbit. It is recommended to mince the meat several times or chew it thoroughly and slowly.
- Low-fat fish: cod, hake, pink salmon;
- Vegetable purees, grated vegetables: potatoes, carrots, beets, young peas;
- Fruit purees, jelly, compotes: strawberries, raspberries, apples;
- Porridges that boil well in water (semolina, oatmeal, rice)
- Milk, fresh low-fat cottage cheese;
- Freshly prepared cabbage juice;
- It is recommended to take alkaline mineral waters (Borjomi): one glass an hour before meals.
- It is necessary to pay special attention to the intake of protein foods - proteins serve as a framework for the formation of new cells.
All food should be minimally seasoned and salted. Food intake is carried out in small portions at certain intervals (5-6 times a day).
Treatment methods
After identifying gastritis, the doctor determines methods of treatment. Self-medication in this case is dangerous due to degeneration into peptic ulcer or stomach cancer. To eliminate this pathology, as a rule, complex treatment is required, which includes following a diet, lifestyle adjustments and taking medications.
Diet features
Properly adjusted nutrition will help eliminate the manifestation of acute gastritis. You can drink without restriction, but it is better to give preference to tea and Borjomi. After the pain subsides, the doctor may recommend switching to a gentle diet, and after the mucous membrane is restored, gradually expanding the list of products.
Basic recommendations for nutrition during gastritis are as follows:
- Eat food in small portions. The number of receptions must be at least 5.
- Avoid eating processed foods and eating from fast food restaurants.
- If you have gastritis, do not eat chocolate, carbonated drinks, sour drinks and juices, sausages, or baked goods.
- Food should be moderately warm. Hot and ice-cold foods and drinks should be avoided.
- During treatment, the menu should not contain fried, spicy or smoked dishes. Dry food should also be avoided.
- Do not eat food with large amounts of salt, spices, sugar, garlic and onions. Drinks containing caffeine should also be avoided for a while.
- The basis of the diet should include lean varieties of meat, poultry and boiled fish, low-fat cottage cheese, vegetable soups and purees, steamed omelettes and other protein foods.
- Among drinks, preference should be given to milk, jelly, fruit compotes and tea.
- It is not recommended to snack on sweets, crackers, or sandwiches.
- The last meal should be no later than 2-3 hours before bedtime.
Drug treatment
In addition to an adjusted diet, it is necessary to treat gastritis of the stomach with medications aimed at:
- normalizing stomach acidity;
- restoration of the condition of the mucous membrane and its protective functions;
- elimination of Helicobacter pylari, if it was previously detected;
- normalization of gastrointestinal motility.
To normalize the acidity of gastric juice, PPIs (proton pump inhibitors) are prescribed. This medicine can normalize the pH level for 20-22 hours. Its action is also aimed at the amount of hydrochloric acid produced.
This group of medicines includes:
- Rabeprazole;
- Omeprazole;
- Lanzoprazole.
Antacids are prescribed to reduce stomach acidity. Their effect on the body lasts no more than 8 hours. Such drugs are not suitable for systematic use and are prescribed only by the attending physician, since they have many contraindications.
Table. Classification of antacids.
| Group name | Effect of drugs | Drug names |
| Suction | They have a short-term effect. After their withdrawal, the production of hydrochloric acid in the stomach increases. Used for temporary relief of gastritis symptoms (heartburn, pain). With long-term use, the following consequences are possible:
|
|
| Non-absorbable |
|
Taking medications is the main method of treating atrophic and erosive gastritis. Only a gastroenterologist can determine a treatment regimen and prescribe medications after a detailed examination.
To normalize gastrointestinal motility, the doctor may prescribe prokinetics. Most often these are tablets of the drug Motilium. In the fight against the Helicobacter bacteria, the doctor may require complex treatment with antibacterial drugs, PPIs and other means.
ethnoscience
Inflammatory processes in the mucous membrane can also be treated with folk remedies. Effective recipes for normalizing the functioning of the stomach and restoring its walls are:
- Infusion of watercress leaves
. It can be used to relieve pain, as well as in advanced forms of gastritis. To prepare it you will need to take 100 g of lettuce leaves, chop and pour in 0.5 liters of boiling water, cover with a lid and leave for a day. The finished infusion is filtered and taken orally, 100 ml twice a day before meals. - Thyme tincture
. To prepare it, take 2 tbsp. dry plant and pour in 0.5 liters of white wine and cover tightly with a lid. It is necessary to infuse the composition for a week in cold conditions. After the time has passed, the mixture is placed on low heat and brought to a boil. Should be taken 2 tsp. before every meal. - Propolis
. In the chronic form of the disease, eating propolis helps. This natural product must be eaten and chewed thoroughly every day, 10 g. - Liquorice root
. An infusion of this root has worked well for gastritis with high stomach acidity. To prepare it, you need to take about 10 g of crushed root, pour it into a thermos and pour 1 liter of boiling water. Leave for 24 hours, strain and take 100 ml before each meal. The duration of the course is 2 weeks. - Potato juice
. The juice from this root vegetable helps relieve the symptoms of gastritis. To prepare it, you will need to take 2 tubers and squeeze the juice out of them. It is recommended to drink it an hour before breakfast. - Honey solution
. To prepare this tasty and simple solution you will need to take 2 tbsp. honey and dissolve it in a glass of warm water. Drink no more than 250 ml of this sweet medicine in one day. Continue the course for up to two weeks. - Herbal collection
. To obtain it, take dried chamomile, yarrow and celandine, place it in an enamel container and pour in 1 liter of boiled milk. The container is carefully closed with a lid and infused for at least 2 hours. The resulting decoction is filtered and drunk in small sips in one day. - Flax seed decoction
. To obtain it at home you will need 2 tbsp. flax seeds and chamomile flowers. The ingredients are placed in a thermos, 1 liter of boiling water is poured in and the lid is tightly closed. The composition is infused for 10 hours, after which it is filtered and taken 400-500 ml per day.
Gastritis cannot be cured in a short period of time. Diet, medication, lifestyle adjustments, all this takes more than one day or even a month. That is why it is better to prevent gastritis: eat little and often, balance your diet, give up bad habits and do not overload your stomach. It is much easier to prevent any disease than to treat it.
What can you drink?
Let's look at some common drinks:
- Milk is easily digestible and reduces stomach acidity. However, milk should not be used as a remedy - only as an addition to solid food. The thing is that milk, being liquid, does not stay in the stomach for a long time, reducing acidity for a short time, it stimulates the secretion of gastric juice to a greater extent.
- Weak tea - it is advisable to drink it when the tea has cooled and become warm.
- Juices – it is advisable to exclude acidic juices: orange, grapefruit, apple, grape. Preference should be given to juices with pulp: peach, banana, apple, pear, tomato. It is not advisable to drink juices chilled; it is better to drink them warm or at room temperature.
- Kissel – partially neutralizes the acidity of gastric juice. However, it should not be consumed as a medicine, only as part of the main meal.
- Mineral waters - preference should be given to alkaline mineral waters: “Essentuki No. 17”, “Essentuki No. 4” and “Semigorskaya”, “Borjomi”.
Is it possible to completely cure gastritis?
You can cure gastritis only if you follow a few simple rules:
- Fractional meals - small portions at least 4 times a day;
- Diet;
- Avoiding smoking;
- Timely use of medications;
- Elimination of stress, physical or psycho-emotional overload;
- Elimination of all types of alcohol;
- A rational regime of work and rest (sleep at least 7 hours a day at night).
Also, any alcoholic drinks for gastritis (especially acute or exacerbation of chronic) are strictly prohibited. Alcohol affects gastric mucus, which protects mucosal cells from the damaging effects of gastric juice. By consuming alcohol, you contribute to greater chemical damage to the stomach lining.