Functional disorders of the gastrointestinal tract constitute a group of heterogeneous (different in nature and origin) clinical conditions, manifested by various symptoms from the gastrointestinal tract and not accompanied by structural, metabolic or systemic changes. In the absence of an organic basis for the disease, such disorders significantly reduce the patient’s quality of life.
To make a diagnosis, symptoms must exist for at least six months with active manifestations for 3 months. It should also be remembered that the symptoms of gastrointestinal tract can overlap and overlap each other in the presence of other diseases not related to the gastrointestinal tract.
Causes of functional disorders of the gastrointestinal tract
There are 2 main reasons:
- Genetic predisposition. FGITs are often hereditary. This is confirmed by the frequent “family” nature of violations. During examinations, genetically transmitted features of the nervous and hormonal regulation of intestinal motility, the properties of receptors in the walls of the gastrointestinal tract, etc. are found to be similar in all (or across generations) family members.
- Mental and infectious sensitization. These include acute intestinal infections, difficult conditions of a person’s social environment (stress, misunderstanding from loved ones, shyness, constant fears of various nature), physically difficult work, etc.
Main manifestations of gastrointestinal tract (GIT) dysfunction
The digestive system is one of the most important systems of the body. The main functions of the gastrointestinal tract: digestive (grinding food, digesting, absorbing and removing excess); barrier (protection of the body from penetration of harmful substances, toxins, allergens, microbes into the blood); immune (participation in the general immune response and local reactions); metabolic (participation in the metabolism of vitamins and microelements). When malfunctions occur in the gastrointestinal tract, these functions are disrupted. If the cause of the failure is not an anatomical factor, then they talk about functional disorders.
The causes of functional disorders of the gastrointestinal tract are: intestinal dysbiosis; disturbances in the functioning of the upper sections, which include the liver, bile ducts, and pancreas; foci of chronic infection in the gastrointestinal tract (including parasites, Giardia, Helicobacter pylori); weakening of the immune system.
We can name the main manifestations of gastrointestinal dysfunction
Secondary lactase deficiency. Very common in children of the first year of life. Associated with immaturity of enzymatic systems and dysbiosis. It manifests itself as bloating, anxiety, loose foamy stools, and sometimes constipation. To identify this condition, it is necessary to take a fecal test “for carbohydrates”, as well as for dysbacteriosis. Dyspepsia syndrome. There are upper dyspepsia with symptoms: nausea, vomiting, belching, heartburn, epigastric pain, heaviness in the abdomen after eating, rapid satiety, bad breath. Manifestations of lower dyspepsia are: flatulence (increased gas formation), stool disorders (unstable, constipation or diarrhea), pain in the lower abdomen. Dyspepsia can occur at any age; only preschool children do not know how to differentiate the location of pain and always point to the navel area. In adolescents and adults, the diagnosis “Irritable Bowel Syndrome - IBS” is used to designate symptoms of dyspepsia. In cases of dyspepsia, it is recommended to take tests: stool for dysbacteriosis, stool for scatology, ultrasound of the abdominal organs, blood for antibodies to Giardia, in adolescents and adults, and blood for antibodies to HP (Helicobacter pylori). Allergic diseases. Nowadays, almost no one doubts the “intestinal” origin of allergic problems, ranging from skin rashes (“diathesis”, allergic dermatosis, food allergies, urticaria, atopic dermatitis) and ending with hay fever and bronchial asthma. In addition to gastrointestinal dysfunction, the causes of allergies are immune dysfunction, as well as the presence of foci of chronic infection both in the gastrointestinal tract and outside it, for example in the respiratory tract. If you have allergic problems, you need to take the same tests as for dyspepsia, plus additional blood for total IgE, for allergens, for opportunistic infections (chlamydia, mycoplasmosis, ureaplasmosis, HSV, CMV, trichomoniasis), as well as a throat smear (bacterial culture) . For children of the first year, it is most often enough to undergo a stool test for dysbacteriosis, since at this age this is the main reason for the development of allergic problems. It should be noted that manifestations of intestinal dysfunction, in addition to the main ones, include such symptoms as: problems with weight gain (both low weight gain and excess weight); problems with appetite; weakened immunity - frequent colds; some neurological or psychological problems - teeth grinding, moodiness, irritability, increased fatigue, mood swings, restless night sleep. Recurrent urinary tract infections may also be associated with intestinal dysfunction. In all these cases, examination of gastrointestinal function and consultation with a gastroenterologist is required.
Symptoms of functional gastrointestinal disorders
Depends on the type of functional disorder:
- Irritable bowel syndrome (large and small) is a functional disorder characterized by the presence of abdominal pain or abdominal discomfort and combined with disturbances in defecation and transit of intestinal contents. To be diagnosed, symptoms must have existed for at least 12 weeks within the past 12 months.
- Functional bloating. It is a frequently recurring feeling of fullness in the abdomen. It is not accompanied by a visible enlargement of the abdomen and other functional gastrointestinal disorders. A bursting feeling should be observed at least 3 days a month for the last 3 months.
- Functional constipation is an intestinal disease of unknown etiology, manifested by constantly difficult, infrequent bowel movements or a feeling of incomplete release of feces. The dysfunction is based on a violation of intestinal transit, the act of defecation, or a combination of both at the same time.
- Functional diarrhea is a chronic syndrome with relapses, characterized by loose or unformed stools without pain and discomfort in the abdomen. It is often a symptom of IBS, but in the absence of other symptoms, it is considered as an independent disease.
- Nonspecific functional bowel disorders - flatulence, rumbling, bloating or distension, a feeling of incomplete bowel movement, transfusion in the abdomen, an imperative urge to defecate and excessive discharge of gases.
Functional disorders of the intestines and biliary tract. Therapeutic approaches, choice of antispasmodic
Functional disorders of the digestive system include various stable combinations of chronic or recurrent gastrointestinal symptoms that are currently not explained by structural, organic or known biochemical pathology.
According to the recommendations of the Rome Consensus III (2006), functional disorders of the intestine and biliary tract include [1]:
I. Functional intestinal disorders:
- irritable bowel syndrome (IBS);
- functional constipation;
- functional diarrhea;
- functional flatulence;
- functional abdominal pain.
II. Dysfunctional disorders of the biliary tract:
- bile duct dysfunction;
- sphincter of Oddi dysfunction.
Based on the nature of motor disorders of the biliary tract, they are divided into hyperfunctional and hypofunctional.
Common clinical manifestations in various forms of functional disorders of the biliary system and intestines are: abdominal pain, flatulence, changes in the frequency and nature of stool.
The parasympathetic and sympathetic parts of the autonomic nervous system take part in the regulation of motor activity of the intestine and biliary system, ensuring their balanced influence with subsequent transmission of impulses to the intramural plexuses.
Contraction of smooth muscle of the gastrointestinal tract (GIT) occurs when acetylcholine stimulates muscarinic receptors on the surface of the muscle cell. This leads to the opening of sodium channels and the entry of Na+ into the cell. The resulting depolarization of the cell, in turn, promotes the opening of calcium channels and the entry of Ca2+ into the cell. The increased intracellular Ca2+ level promotes myosin phosphorylation and, accordingly, muscle contraction. Depending on the intensity of the signal, muscle spasm may occur, which causes pain.
In turn, sympathetic impulses promote the release of K+ from the cell and Ca2+ from the calcium store, the closure of calcium channels and muscle relaxation [2, 3].
Thus, given the fact that the formation of pain in biliary dysfunction and functional intestinal disorders is due to excessive contraction of smooth muscles, antispastic drugs should occupy the main place in their relief.
Currently, smooth muscle relaxants are used to relieve pain, which include the following groups:
1. Myotropic antispasmodics:
- ion channel blockers: selective calcium channel blockers (Dicetel);
- sodium channel blockers: mebeverine (Mebeverine hydrochloride, Duspatalin);
- isosorbide dinitrate;
2. Neurotropic antispasmodics (block the process of transmission of nerve impulses in the autonomic ganglia and nerve endings that stimulate smooth muscle cells):
- natural (atropine, hyoscineamine, belladonna preparations, platiphylline, scopolamine);
- synthetic and semi-synthetic central (adifenin, aprofen, Aprenal, cyclosil);
- semisynthetic peripheral (hyoscine butyl bromide - Buscopan).
3. Prokinetics - a group of drugs that normalize the motor activity of the gastrointestinal tract; enhance the propulsive activity of the upper gastrointestinal tract due to antagonism with dopamine receptors (metoclopromide, domperidone (Motilium) and itopride (Ganaton), which, in addition to blocking dopamine receptors, inhibits the activity of cholinesterase, suppressing the destruction of acetylcholine, expanding the regulatory zone).
4. Universal modulators of gastrointestinal motility (blockers of µ-, δ-receptors and activators of κ-receptors) - trimebutine (Trimedat).
Thus, functional disorders of the gastrointestinal tract are based on motility disorders, and the group of drugs presented above in one way or another affects tonic-peristaltic activity, and the range of these effects is very diverse and often, using them, we are faced with effects that are undesirable in this particular situation. Thus, neurotropic antispasmodics have a wide range of “side” effects that limit their long-term use, and in certain categories of patients their use is generally inappropriate. The main disadvantage of myotropic antispasmodics is the lack of selectivity and the possibility of developing hypomotor dyskinesia and hypotension of the entire sphincter apparatus of the gastrointestinal tract [4].
Summarizing all of the above, we can state that today we have a large arsenal of drugs that act on different pathogenetic links of smooth muscle spasm that form pain. Our task is to choose the most adequate antispasmodic, minimize side effects, relieve pain as quickly as possible, limit it, and prevent its return.
Why is pain the main manifestation that determines the choice of drug? Because it is often the only symptom indicating a functional disorder, and other manifestations require evidence-based examination.
How to choose the most rational drug for treatment? We offer the following drug selection algorithm:
I. Depending on the severity and area of distribution of the antispasmodic effect (Table 1).
II. Depending on the combination of spasm zones:
a) stomach + genitourinary area; b) esophagus, stomach + intestines; c) esophagus + bladder; d) bile ducts + ureters (kidneys); e) biliary tract; f) intestines (without specific location); g) intestines (right sections); h) intestines + sphincter of Oddi; i) “spastic dyskinesia” + prostate pathology; j) spastic dyskinesia + elderly and senile age.
III. Depending on the intensity of pain (acute - parenteral version of the drug).
IV. Depending on age.
V. Depending on the costs of using antispasmodics:
a) “erasing” symptoms; b) distribution of coverage areas; c) negative effects when combined with other pharmaceuticals; d) a variant of the initial state of the autonomic nervous system.
The proposed algorithm for choosing a drug is not a dogma - it only shows guidelines that help in the choice. Having chosen and started treatment, we evaluate the effectiveness of:
- if the effect is sufficient, we continue treatment;
- if there is an effect, but it is insufficient, we change the dose, having achieved an effect, we continue treatment;
- in the absence of sufficient effect and maximum doses, we proceed to combined treatment (another group of drugs, their combination, combined treatment option).
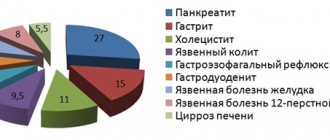
But the main thing in treatment is the diagnosis of the “clinical situation”, which allows us to talk about either organic pathology and the secondary nature of functional disorders, or about functional pathology (Fig.).
Thus, the diagnosis of functional pathology today is a diagnosis of excluding organic pathology. Having established this, we assess the nature of functional disorders and define the complex of disorders as a whole.
We decided to present the results of treatment of 60 patients with Dicetel: 30 of them suffered from irritable bowel syndrome (10 each with constipation, diarrhea, pain and bloating). The age of patients is from 18 to 60 years; Women prevailed - 2:1. Diarrheal syndrome was characterized by the absence of diarrhea at night; the urge to stool occurred in the morning, after breakfast, stool was preceded by pain of a “spastic” nature, which disappeared after stool. Constipation was constant (in 8 patients); in 2 patients it was periodic. The variant of IBS with pain and bloating in 7 patients was of a constant nature, in 3 - the character of paroxysmal bloating.
The study excluded organic pathology (irrigoscopy, colonoscopy). Control of motor skills was: electromyography, “carbolene test” in dynamics. Treatment with Dicetel was carried out for 4 weeks at a daily dose of 150 mg. If the effect was assessed as insufficient, the dose could be increased to 300 mg/day; if it was not possible to cope with diarrhea, then the treatment was supplemented with Smecta; if constipation could not be managed, then Forlax was prescribed. The effectiveness of treatment was assessed by the dynamics of clinical symptoms, the speed and completeness of pain relief.
Treatment results
During Dicetel therapy for 2 weeks, the overall effectiveness was 63% (pain was completely relieved in all patients). Constipation was mainly relieved at a dose of 150 mg/day - in 77% of patients; in 5 patients, an increase in the dose of Dicetel was required to 300 mg/day and in one patient the prescription of Forlax was required. In the variant with diarrhea, the effect was 74%, in 5 patients (15%) the prescription of Smecta was required, although the total number of relaxations decreased to 1–2 times a day; In 1 patient, imperative urges disappeared, although morning (loose, semi-formed) stools remained. When studying the “carbolene test,” an increase in the passage time through the intestines was recorded from 14.3 hours to 18.1 hours. In the group of patients with pain and flatulence, during the first two weeks of treatment, a decrease in the degree of bloating and pain was achieved in 63% of patients, and only increasing the dose of Dicetel to 300 mg/day led to regression of symptoms in 83% of patients; 17% of patients required drug correction of dysbiosis, and only after this the full effect was achieved in 87% of patients (4 patients retained a moderate degree of bloating, constant or paroxysmal).
Thus, the use of Dicetel for the treatment of patients with IBS (various variants) at a dose of 150 mg/day turned out to be effective in 63% of patients, increasing the dose of the drug to 300 mg/day made it possible to achieve an overall effect in 77% of patients; 17% of patients required a combined treatment option (Smecta in patients with weakness; Forlax in patients with constipation and Baktisubtil in patients with bloating and pain).
In 2 patients (6%), a sufficient effect was not obtained, and we examined them in terms of a more complex genesis of functional disorders, although the pain decreased significantly.
The second group consisted of 30 patients aged from 20 to 74 years with various biliary dyskinesias. 10 patients had hypokinetic dyskinesia of the gallbladder (HGBD), 10 had sphincter of Oddi dysfunction type 3 (SDO), 10 had hyperkinetic dyskinesia of the gallbladder (HGD). The average age of the patients was 54.6 years. There were 3 men, 27 women.
All patients complained of pain of various types, dyspeptic symptoms and intestinal disorders. The pain was localized mainly in the right hypochondrium, did not radiate, was provoked by food, and the intensity was moderate.
The results of the study of dyspeptic syndrome and the nature of stool are presented in table. 2.
As can be seen from the table, dyspeptic manifestations were recorded in 70% of patients (with different frequencies in different groups, maximum in patients with hypokinesia of the gallbladder and DSO) and in almost half of the patients certain stool disorders were recorded.
Patients randomized into groups received Dicetel monotherapy at a daily dose of 50 mg × 3 times. The total duration of treatment was 20 days.
Treatment results
- Positive dynamics in relation to pain syndrome were noted in 83% of patients (in 17% the pain decreased, but did not completely go away); at the same time, in patients with HDZhP and GrZhP - on average by the 5th day, and in patients with DSO - by the 10th day.
- Dyspeptic syndrome: nausea stopped by the 4th day in patients with DSO; by 5–6 days in patients with ADHD; – by the 7th day in patients with HDJP;
- flatulence - completely stopped by 7-8 days in 7 patients, in 4 patients it persisted in a low degree and only after eating.
In general, a positive effect on dyspeptic syndrome was achieved in 80% of patients.
Normalization of intestinal function both with constipation (6 patients) and with streaks (5 patients) occurred by 10–14 days of treatment in all patients.
Among the side effects, 2 patients experienced increased pain in the upper abdomen - in one case at the beginning of treatment, and in the other on days 6–9 of treatment, which was the reason for discontinuation of the drug.
Thus, a positive effect regarding pain syndrome was obtained in 83% of cases, dyspeptic syndrome in 80% of cases and intestinal dysfunction syndrome in 100% of cases.
The effect of Dicetel on the condition of the gallbladder was also assessed, and a predominant effect of the drug on hypertonicity of the gallbladder and restoration of normokinesia in 80% of patients was noted, which is most likely due to the restoration of the pressure gradient and normalization of gallbladder emptying in this regard.
When assessing the effect of Dicetel on functional intestinal pathology (IBS) and biliary dyskinesia, based on the study, the effect should be noted in 80% of patients. This is a good indicator, while a small number of “side” effects are recorded, which is most likely due to the selective effect of its action, which is realized only at the intestinal level. The lack of effect in a certain category of patients can be enhanced by the dose (maximum doses were not used) or a combined treatment option for individual symptoms of intestinal dyspepsia.
The lack of effect in a small proportion of patients (6–10%) is most likely due to a violation of other regulatory systems (opioid, autonomic nervous system, hormonal system), which must be used in cases of treatment failure.
Conclusion
This report presents data on functional disorders of the intestines and biliary tract, as well as medications that affect the tone and contractility of the gastrointestinal tract. Based on our own data, we proposed an algorithm for choosing a drug that affects dysfunctional disorders and the results of treatment of patients with different types of IBS and dysfunctional biliary tract disorders (60 patients in total). A representative of myotropic antispasmodics, the selective calcium channel blocker Dicetel, was used in the treatment. The drug has been shown to be highly effective in treatment (83% effective in the treatment of IBS and 80% effective in the treatment of functional disorders of the biliary tract).
The selectivity of the drug ensured a small number of side effects (3.3%). In relation to intestinal dysfunction, the drug has a direct antispasmodic effect; in relation to biliary tract dysfunction, it has a predominantly indirect effect associated with a decrease in intraluminal pressure in the intestine, restoration of the pressure gradient and passage of bile. The drug may be recommended for the treatment of these disorders.
Literature
- Drossman DA The Functional Gastrointestinal Disorders and the Rome III Process // Gastroenterology. 2006; 130(5):1377–1390.
- McCallum RW The role of calcium and calcium antagonism in motility disorders of the gastrointestinal tract. In: Calcium antagonism & Gastrointestinal motility // Experta Medica. 1989, p. 28–31.
- Wesdorp ICE The central role of Ca++ as mediator of gastrointestinal motility. In: Calcium antagonism & Gastrointestinal motility // Experta Medica. 1989, p. 20–27.
- Makhov V.M., Romasenko L.V., Turko T.V. Comorbidity of dysfunctional disorders of the digestive organs // Breast Cancer. 2007, vol. 9, no. 2, p. 37–41.
O. N. Minushkin, Doctor of Medical Sciences, Professor
FSBI UMTS Administrative Department of the President of the Russian Federation, Moscow
Contact information about the author for correspondence
Treatment of functional gastrointestinal disorders
Complex treatment includes dietary recommendations, psychotherapeutic measures, drug therapy, and physiotherapeutic procedures.
General recommendations for constipation: abolition of constipation medications, foods that contribute to constipation, intake of large amounts of fluid, food rich in ballast substances (bran), physical activity and elimination of stress.
If diarrhea predominates, the intake of coarse fiber into the body is limited and drug therapy (imodium) is prescribed.
If pain predominates, antispasmodics and physiotherapeutic procedures are prescribed.