Description
Gastric bleeding is one of the most common conditions that occurs against the background of various diseases of the stomach and duodenum. At the same time, venous or arterial blood flows freely into the lumen of the stomach. The volume of lost blood can reach 3-4 liters, and therefore the prognosis for gastric bleeding is not always favorable, and in the absence of therapeutic measures it can lead to the death of the patient.
Classification of gastric bleeding
Today, there are many principles for dividing gastric bleeding into different groups.
Due to the occurrence:
- Ulcerative bleeding – the source of bleeding is chronic and acute gastric ulcers of any location;
- Non-ulcer bleeding – the causes of bleeding are varied, you can read about them below.
According to the nature of the flow:
- Ongoing: Smooth or profuse,
- Capillary,
- Recurrent,
- Unstable;
According to the severity of the clinical picture:
- Mild severity – vomiting once or twice, darkening of the stool, changes in blood pressure and pulse are not observed. Full compensation for the condition.
- Moderate severity – vomiting more than once, decreased blood pressure: systolic to 90 mm Hg. Art., slight tachycardia - pulse up to 100 beats per minute. Relative compensation of the condition.
- Severe severity - repeated vomiting of blood, non-stop, drop in blood pressure: systolic up to 60 mm Hg. Art. and lower, significant tachycardia - up to 120 beats. per minute with a possible transition to bradycardia (pulse less than 60 beats). Decompensation of the condition.
According to the endoscopic picture:
- IA – blood flows from the site of injury in a stream;
- IB – drip bleeding from damage to the mucous membrane;
- IIA – a thrombosed vessel is observed at the bottom of the ulcer;
- IIB – the ulcer is closed by a blood clot;
- IIC – an ulcer without signs of bleeding is observed;
- III – the source of bleeding cannot be detected.
In addition, there is a division of gastric bleeding into:
- Acute and chronic, differing in the time of bleeding;
- Hidden and obvious, characterized by the absence or presence of corresponding clinical symptoms in a person;
- Single and recurrent, divided by frequency of bleeding.
Causes of stomach bleeding
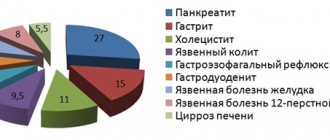
Today, more than 100 possible causes of gastric bleeding can be identified. Let's talk about the most common among them.
The first large group of reasons is associated with the pathology of the stomach itself.
Stomach ulcer. In 10-20% of cases, this disease is characterized by the development of gastric bleeding. In this case, the mechanism of bleeding can be different: either direct damage to the vessel occurs due to the aggressive contents of the stomach, or the vessel ruptures due to a blood clot formed in it.
Malignant neoplasms of the stomach. They are characterized by constant growth deep into the wall of the organ with possible damage to the integrity of the blood vessels. Stomach cancer can be either a separate disease or develop against the background of a peptic ulcer.
Diverticular disease and isolated diverticula. In this case, small “finger-like” protrusions are formed in the wall of the stomach. Against the background of damaging factors, inflammation of the diverticulum occurs - diverticulitis (with the risk of damage to the vessels of the organ wall in this place).
Diaphragmatic hernia. The disease is characterized by weakness of the diaphragm and movement of part of the stomach into the chest cavity through the esophageal opening of the diaphragm. Bleeding can occur either due to the constant effect of stomach hydrochloric acid on the thin mucous membrane of the esophagus, or due to the formation of stomach ulcers at the junction of the stomach with the chest cavity.
Polyps in the stomach. A polyp is a benign tumor of the gastric mucosa. Damage to blood vessels can occur due to the formation of an ulcer on the polyp, trauma and formation, or local circulatory disorders in the polyp.
In addition to causes related to the stomach, there is a large group of diseases of other organs that can also lead to the development of gastric bleeding.
Portal hypertension with varicose veins of the esophagus and upper stomach. At the bottom of the esophagus there is a very large venous plexus - this is the junction of veins from two different venous systems. These veins lie very superficially and can be easily injured, especially against the background of diseases associated with their expansion: hepatitis of the liver resulting in cirrhosis, tumors of the liver and biliary tract, portal vein thrombosis, portal vein compression syndromes in various pathologies.
Systemic vasculitis with damage to blood vessels of any location (including gastric). With these diseases, damage to the inner lining of the blood vessels occurs, which leads to their increased fragility and frequent ruptures.
Pathology of the blood coagulation system leads to an increased risk of bleeding from any location, including from the vessels of the stomach. Any microtrauma against the background of these diseases can lead to serious gastric bleeding.
Causes of stomach bleeding in children
The causes of gastric bleeding in children differ from those typical for adults and vary depending on the age of the child:
- In newborns, the most common cause of gastric bleeding is hemorrhagic disease of the newborn, associated with a lack of vitamin K and a violation of the synthesis of blood clotting factors as a result.
- In children from 1 to 3 years of age, gastric bleeding most often occurs due to various intussusceptions, diverticula and diaphragmatic hernias of the stomach.
- In children aged 3 to 7 years, the most common cause is gastric polyposis, which occurs as a hereditary disease.
In addition, a common cause of gastric bleeding in children are various infectious diseases affecting the gastrointestinal tract (salmonellosis, dysentery, etc.), injuries and foreign bodies entering the stomach.
Complications of gastric bleeding
The most common complications of ongoing gastric bleeding are posthemorrhagic anemia and hemorrhagic shock.
Posthemorrhagic anemia is characterized by a decrease in the level of hemoglobin and red blood cells in the patient and is associated with a constant loss of hemoglobin and extravascular destruction of red blood cells. Does not pose a serious threat to health if corrected in a timely manner.
Hemorrhagic shock develops against the background of massive blood loss and is characterized by a drop in blood pressure, the development of acute cardiac and pulmonary failure and kidney damage due to their hypoxia. The condition poses a mortal danger to the patient and requires immediate assistance from the resuscitation team.
Therefore, if any symptoms of gastric or gastrointestinal bleeding appear, it is necessary to immediately contact a specialist in a medical institution to carry out diagnostic measures and organize rational treatment.
Causes of stomach bleeding
Gastric bleeding is a complication of various chronic and inflammatory diseases.
Hemorrhage, or in other words hemorrhage, is often caused by a duodenal ulcer. If left untreated, the inflammatory process of the gastric mucosa leads to bleeding. The cause of gastric bleeding is the appearance of benign or malignant neoplasms. Increased pressure in the intestines leads to gastrointestinal disorders, including bleeding of internal organs.
Hiatal hernias, like tumors, are accompanied by hemorrhage and lead to death if undiagnosed. The pathology can be caused by ulcerative colitis, hemorrhoids, or anal fissures. Occurs against the background of liver cirrhosis, dysbacteriosis, pancreatitis. Diseases such as hepatitis B, C, vein thrombosis, and hypertension also lead to bleeding.
Bleeding occurs when veins are pressed by tumors and scars. The cause of gastric bleeding can be damage to blood vessels, varicose veins of the stomach and intestines, lupus erythematosus, vitamin deficiency and reduced immunity. This pathology often occurs due to circulatory disorders. For example, hemophilia, acute and chronic leukemia, hypoprothrombinemia. Bleeding is also caused by excessive intake of aspirin, alcohol or drug intoxication, overdose of drugs and chemicals. Depression and constant emotional stress can affect such symptoms.
Gastric bleeding is caused by vascular abnormalities. We are talking about erosion, thrombosis and rupture of capillaries. The cause is called a change in the hemostatic system when blood clotting is impaired.
Symptoms
Photo: om1.ru
Gastric bleeding is a serious complication of a number of diseases of the stomach and other organs of the human body, characterized by the outpouring of venous or arterial blood into the lumen of the stomach.
Symptoms of gastric bleeding are varied and depend on a number of factors: the disease against which the bleeding developed; volume and duration of blood loss. At the same time, certain patterns can be identified in the development of the clinical picture and the symptoms can be divided into several groups.
General symptoms of blood loss
The first signs of gastric bleeding are the appearance in the patient of gradually increasing general weakness, lethargy, and a decrease in physical and intellectual performance. Further blood loss leads to the development of symptoms of stage 1 hemorrhagic shock: a person experiences dizziness, attacks of general weakness, becomes pale, cold sticky sweat appears on the forehead and back, tachycardia occurs and a drop in blood pressure occurs (systolic pressure up to 90 mm Hg). In this case, a slight initial mental arousal is possible, which is replaced by apathy and indifference to the environment.
Vomiting and changes in stool
Changes in bowel movements and the appearance of vomiting with certain characteristics are the most important symptoms of gastric bleeding. When bleeding, as a rule, the vomit has the appearance of “coffee grounds” with a brown color and blood clots. If the bleeding is profuse, then the blood may not be changed and be red-scarlet in color.
The next characteristic sign of gastric bleeding is baby-like stool or melena. It is characterized by a black color and is a symptom of bleeding from the upper gastrointestinal tract. It is important to note that it is the appearance of melena in a person that allows one to suspect hidden bleeding from the stomach or small intestine. If there are streaks of scarlet blood in the stool, then the source of bleeding is in the anus.
Symptoms of stomach bleeding in children
The general picture of the development of gastric bleeding in children is similar to that in adults. But due to the fact that children cannot always describe their sensations, some symptoms may go unnoticed.
The appearance of vomiting blood and baby-like stools are characteristic signs of gastric bleeding at any age. In addition, the child experiences lethargy, lack of interest in the things and people around him, pale skin and visible mucous membranes, and cold extremities. As internal bleeding progresses, facial features become sharper, dark circles form around the eyes, the child begins to yawn and tries to go to bed, despite the severity of the condition. Such signs are characteristic of dehydration due to the loss of a large volume of blood.
Very often, gastric bleeding in children is characterized by a hidden course. Then the symptoms of posthemorrhagic anemia come to the fore: weakness, dizziness, increased fatigue during physical and mental work, pallor.
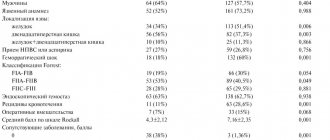
Symptoms in combination with peptic ulcer
Among all the causes of gastric bleeding, ulcers due to gastric ulcers and other conditions occupy a leading place - 60-80% in the structure of causes. At the same time, a number of factors play a great role in the occurrence of ulcers: a person’s diet, medication intake, concomitant pathology, etc. Bleeding from ulcers is usually characterized by massiveness and a high mortality rate. In 15-20% of cases, it is gastric bleeding that is the reason for seeking medical help. Most often, such a complication of peptic ulcer disease occurs in people over 40 years of age with the presence of risk factors (taking non-steroidal anti-inflammatory drugs, smoking, non-compliance with dietary restrictions, etc.). Very often, bleeding precedes or develops simultaneously with perforation of the stomach wall.
The pattern of symptoms for peptic ulcers with bleeding is very specific. Against the background of a painful attack in the upper abdomen, a feeling of weakness, and unpleasant sensations in the mouth, the pain syndrome suddenly goes away and vomiting occurs - either in the form of “coffee” grounds, or in the form of slightly changed blood. If perforation develops during bleeding, then the pain takes on a dagger-like hue, the patient begins to feel severe weakness, dizziness and nervous excitement. Symptoms of peritonitis develop: diffuse pain throughout the abdomen, tension in the anterior abdominal wall, a rise in body temperature to 38-39 degrees. In most cases, this condition is fatal.
It is very important that if any of these symptoms appear, immediately contact a medical institution to receive specialized first aid, carry out diagnostic measures and prescribe treatment for the patient.
Diagnostics
Photo: medhealthservices.com
When the first signs of gastric bleeding appear, you should immediately consult a doctor, since this condition poses a great danger to human life. Emergency care provided to the patient is aimed at eliminating the symptoms and identifying the causes of this condition.
Diagnosis of gastrointestinal bleeding includes:
- endoscopic examination;
- X-ray of the stomach;
- vascular angiography;
- radioisotope scanning;
- capsule endoscopy;
- colonoscopy;
- Magnetic resonance imaging;
- blood test;
- coagulogram;
- rectal and external examination;
- stool analysis for the presence of hidden bleeding.
Differential diagnosis of gastric bleeding also includes an analysis of factors that could provoke the disease. The person’s lifestyle and what medications he or she takes must be taken into account. The patient’s medical record must be studied to determine the presence of concomitant diseases that could cause the main signs of gastric bleeding.
Clinical examination
Examination of a sick person must include the following:
- examination of the condition of the skin. This takes into account the presence of hematomas, dilated small vessels and other factors that may affect the correct diagnosis;
- digital examination of the rectum, which helps to identify the presence of bleeding. Also, this diagnostic method is necessary to assess the patient’s condition, to identify tumors or hemorrhoids;
- palpation of the abdominal cavity, which reveals possible enlargement of the liver or spleen, accumulation of fluid, and the appearance of various neoplasms;
- determining the size of lymph nodes.
When gastrointestinal bleeding occurs, a change in stool occurs, so a stool analysis is required. This may indicate the location of the problem - in the stomach, intestines, or rectum.
A clinical study is not able to identify the causes of bleeding, but it may well determine the severity of the patient’s condition and the degree of blood loss. The diagnosis is also influenced by the presence or absence of pain during palpation of the abdominal cavity.
Laboratory research
Diagnosis of gastric bleeding necessarily includes a number of laboratory methods:
- General blood test - determines the amount of hemoglobin, red blood cells, leukocytes, platelets, ESR. These data may change for the worse even after bleeding has stopped;
- coagulogram - determination of blood clotting disorders. It is carried out using special equipment, where several indicators are analyzed that indicate the presence of pathologies;
- biochemical analysis - reveals the amount of urea, creatine in the blood and determines other equally important data that directly affects the diagnosis and treatment tactics.
These analyzes are of great value if they are performed several times. The main indicators that are visible over time indicate the course of the disease and the effectiveness of treatment.
Endoscopic examination
A comprehensive diagnosis of gastric bleeding necessarily includes examination using a fibrogastroscope, at the end of which there is a small camera. This allows the gastroenterologist to carefully examine the mucous membrane of the esophagus and stomach. This study is very informative and in most cases determines the source of bleeding in the digestive system.
Endoscopy is performed as follows:
- The person lies on his left side.
- An anesthetic spray is used to numb the mucous membrane.
- A special mouthpiece is placed in the patient's mouth.
- The doctor inserts a special device through the person’s mouth into the stomach - a fibrogastroscope, which is a flexible cord. During this time, the patient should not move and breathe intensively through the nose.
This study is quite unpleasant, but it takes a little time and is very informative.
X-ray of the stomach
How to determine gastric bleeding? In many cases, an X-ray of the stomach using a contrast agent will be quite informative. Using this study, it is possible to assess the condition of the walls of this organ and identify various pathologies.
X-rays are performed exclusively on an empty stomach. If the stomach is filled with food, the contrast agent will not be able to distribute properly throughout its walls.
Research methodology:
- The person should drink a solution containing barium sulfate. A special feature of this substance is that it does not transmit x-rays.
- Several x-ray pictures are taken. In this case, the person must take different positions so that the study is as informative as possible.
- An analysis of x-rays is carried out, on which the stomach is clearly visible.
Angiography
Angiography or X-ray contrast examination is indicated when there is a suspicion that gastric bleeding is caused by vascular pathology. This may be caused by atherosclerosis or other serious disorders.
This study is carried out using a special contrast agent, which is injected into the vessel using a catheter. After this, an x-ray is taken. The resulting images clearly show the vessel. Based on the data obtained, it is possible to draw conclusions about the cause of gastric bleeding.
Radioisotope scanning
This study is carried out in cases where other diagnostic methods have failed to identify the causes of bleeding.
Before radioisotope scanning, a solution containing red blood cells, which are marked with a contrast agent, is injected into the blood of a sick person. After this, they accumulate in large quantities at the site of bleeding. It can be identified in photographs taken by a special device.
Magnetic resonance imaging
This study is carried out when the doctor needs additional data about the health status of a sick person. Magnetic resonance imaging allows you to obtain a 3D image of a specific organ or images with layer-by-layer sections of the necessary parts of the body.
This study is very informative and is carried out using a special installation - a tomograph.
Colonoscopy – indications and how it is performed
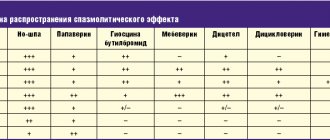
Colonoscopy is considered the most informative method for diagnosing defects of the large intestine. With its help, you can identify pathologies that caused heavy bleeding. The procedure is carried out with a special long probe - an endoscope. It is inserted through the anus into the intestines, after which the doctor sees an image of the mucous membrane on the screen. A significant disadvantage of the method is that a colonoscopy cannot be performed if a person has intense bleeding.
This procedure is quite complex and time-consuming. To avoid discomfort, you must strictly follow all the doctor’s instructions. Before the procedure, you need to completely cleanse the intestines. To do this, you need to take a special drug in the evening if the colonoscopy takes place in the morning. To reduce pain, antispasmodics are also prescribed. For the same purpose, immediately before inserting the probe into the intestines, the doctor injects the patient with an anesthetic.
The procedure does not last long. On average, 10-15 minutes are enough.
Capsule endoscopy is an innovative method for diagnosing gastrointestinal bleeding
In some cases, a doctor may decide to use a modern capsule endoscopy method to diagnose pathologies of the digestive system. It consists in the fact that the patient must swallow a special endocapsule.
This device transmits in real time an image of the mucous membranes of the digestive system. Capsule endoscopy allows you to identify pathologies of the stomach, esophagus, small and large intestines, duodenum, which may have gone unnoticed during other studies.
The duration of the procedure is 8-9 hours. The advantage of diagnosis is that the patient does not need to lie down during this time. A person can do his usual activities. There is also no need to specifically remove the endocapsule. When the device passes through the entire digestive tract, it comes out naturally on its own.
Bleeding from the small intestine (intestinal bleeding of “unclear” etiology)
The main danger is death due to acute or chronic blood loss. The causes of bleeding from the small intestine are disintegrating tumors and malformations of blood vessels in the submucosal layer - angioectasia and angiodysplasia. Patients experience increasing symptoms of chronic blood loss - anemia, weakness, decreased function of all organs.
- Difficulties in diagnosis
Large tumors and large malformations (venous-cavernous forms of angiodysplasia) are detected using a contrast-enhanced CT scan. Diagnosis of other causes of bleeding from the small intestine is extremely difficult, since their source can be very small. Gastroscopy and colonoscopy do not detect the source of bleeding because a standard endoscope cannot penetrate the small intestine. Computed tomography with contrast also does not provide clear information. Symptoms of blood loss increase, and patients undergo multiple blood transfusions to maintain life. A desperate step is to perform a diagnostic laparoscopy, and sometimes an open operation - laparotomy, but these methods almost never detect the cause of the bleeding - a miniature vascular tumor.
- Video capsule enteroscopy
The Ilyinskaya Hospital uses the most modern method for diagnosing bleeding from the small intestine - video capsule enteroscopy. After preliminary bowel preparation, the patient swallows a special video capsule. The capsule contains a camera, a light source and a power source that allows it to operate autonomously for up to 15 hours. A compact video signal receiver connected to the capsule via Bluetooth is placed on the patient’s belt. The capsule is disposable. The doctor receives a clear video image of the entire length of the small intestine. Video capsule enteroscopy allows you to accurately determine the localization of mucosal angioectasia measuring 5–6 mm, which cannot be done by other methods.
- Double balloon intestinoscopy
After the source of bleeding has been identified using video capsule enteroscopy, it is necessary to stop the bleeding and eliminate its cause. For this, surgeons at the Ilyinskaya Hospital use a modern high-tech technique - double-balloon intestinoscopy. The operation is performed under anesthesia. A special flexible and long endoscope - an intestinoscope - is inserted into the small intestine. Alternately inflating two balloons of the intestinoscope, the surgeon moves it along the small intestine to the area with angioectasia and clips the bleeding site. This location is marked using a special contrast agent. Laparoscopic surgery is then performed. Through three small incisions, a laparoscope and surgical manipulators are inserted into the abdominal cavity. The surgeon easily finds the area of angioectasia, marked with contrast, and performs resection of this fragment of the small intestine. The cause of blood loss is radically eliminated.
The use of video capsules and intestinoscopes has fundamentally improved the cure rate of patients with bleeding from the small intestine. The specialists of the Ilyinskaya Hospital are recognized experts in this complex and high-tech field of surgery.
Treatment
Photo: healthy-joint.ru
The pathology poses a serious health hazard due to the high probability of developing severe complications, including death. If signs of gastric bleeding appear, the patient should be put to bed and kept at rest. Eating is prohibited. It is recommended to place a cold compress or ice on the patient's stomach. You should call an ambulance immediately.
Upon admission to the surgical department, strict bed rest is prescribed. Any physical activity is prohibited - this is necessary to reduce the risk of re-bleeding. First, hunger is shown. Subsequently, a special diet is recommended, which must be followed after hemostasis has been achieved.
Drug therapy
Isolated conservative treatment is allowed for minor bleeding, and is often used simultaneously with endoscopic or surgical methods. Indicated in the following situations:
- Minor blood loss that does not pose a threat to human health.
- The presence of severe concomitant diseases (acute and chronic leukemia, malignant neoplasms of various localizations, chronic heart failure in the decompensation phase, etc.);
- Diseases of the hemostatic system that threaten to intensify or develop new bleeding when attempting surgery.
There are three areas of drug therapy for gastric bleeding:
- correction of the hemostatic system;
- impact directly on the source of bleeding;
- restoration of circulating blood volume using infusion therapy.
In addition to the use of medications, the stomach is periodically washed with chilled water, which allows it to be cleared of blood clots and cause a reflex spasm of blood vessels. If the source of bleeding is in the lower esophagus and cardiac part of the stomach, a special Blackmore probe is used to compress dilated and damaged venous vessels. The tube is inserted into the esophagus through the mouth and inflated with air.
All patients with ulcer bleeding should be examined for the presence of Helicobacter pylori bacteria, which cause damage to the mucous membrane. If the test result is positive, it is necessary to prescribe combination antibacterial therapy to eradicate the pathogen.
Endoscopic methods
In modern medicine, methods of endoscopic treatment of gastric bleeding are actively used. As part of minimally invasive interventions, the following are carried out:
- cauterization of a bleeding vessel with electric current;
- local high temperature exposure;
- applying adhesives to the source of bleeding.
In addition, with the help of endoscopic devices it is possible to suturing bleeding vessels in the stomach and esophagus. All manipulations are performed during therapeutic gastroscopy. These techniques have proven to be effective, with minimal risk of side effects.
Surgery
Surgical treatment is indicated for peptic ulcers, severe, massive and recurrent bleeding that cannot be stopped using minimally invasive techniques. Operations can be performed in two ways: laparoscopically (through small incisions on the anterior abdominal wall using an endoscope) or laparotomically (through a wide incision in the abdomen for better access to the stomach).
Possible stitching or excision of the ulcer. In case of extensive organ damage, resection (removal of part of the organ) followed by the formation of an anastomosis may be required. There are many options for resection, involving the connection of the gastric stump with the duodenum or small intestine. The choice of the appropriate technique is made by the surgeon.
X-ray surgical embolization of the gastric artery is considered a promising method for treating peptic ulcers - in this case, a means for blocking blood flow (spiral, microsphere, gelatin sponge, etc.) is brought to the site of the lesion using a special catheter inserted into the vessel on the thigh. No incisions are required in the stomach area.
Bleeding
Bleeding from wounds
Cuts, stabs, bruises, lacerations and puncture wounds are accompanied by an outpouring of blood into the external environment.
The scope of first aid depends on the type of bleeding. In case of arterial bleeding, a tourniquet made of an elastic rubber band is applied to the limb, after placing a strip of fabric folded in several layers under it. It must be taken into account that applying a tourniquet to the lower leg or forearm is ineffective, since the vessels in these segments are located in such a way that it is difficult to “squeeze” them from the outside. Therefore, for wounds of the upper limb accompanied by arterial bleeding, a tourniquet is applied to the shoulder, and for wounds of the lower limb - to the thigh. The wound area is covered with a sterile bandage, the victim is given pain relief and urgently taken to a medical facility. If transportation takes a significant amount of time, it is necessary to periodically loosen the tourniquet, pressing the damaged artery above the wound site. For adults, the maximum time for applying a tourniquet is 1 hour, for children – no more than 20 minutes. For wounds accompanied by venous bleeding, a pressure bandage is applied. For capillary bleeding, a regular sterile bandage is sufficient.
Making a diagnosis for external bleeding is not difficult. The key to diagnosis is to identify damage to internal organs and important anatomical structures. If the bottom of the wound is not accessible for direct inspection, and the localization does not allow to exclude a violation of the integrity of the muscles, joints, natural cavities and internal organs, the patient is referred for additional examination and consultations with the appropriate specialists are prescribed: cardiac surgeon, thoracic surgeon, abdominal surgeon, urologist, etc. If necessary, chest radiography, arthroscopy, laparoscopy, ultrasound, MRI and other studies can be performed.
Patients with damage to internal organs are transferred to the care of specialists of the appropriate profile. Patients with damage to capillaries, veins and small arteries are referred to traumatologists. Vascular surgeons treat wounds with disruption of the integrity of large arterial trunks. On admission, all patients with arterial and venous bleeding undergo a blood test to assess blood loss. Treatment consists of PSO. The operation is performed under local anesthesia or general anesthesia. If large arterial trunks are damaged, sutures are placed on the vessel wall or grafts are used. The scope of surgical interventions in cases of violation of the integrity of internal organs depends on the nature and severity of the injury.
Bleeding from fractures
All fractures are accompanied by bleeding from damaged bone fragments. With open fractures, blood flows outward and into the surrounding tissues, with closed extra-articular fractures - only into the surrounding tissues, with closed intra-articular ones - into the joint cavity. The amount of blood loss depends on the location and type of fracture. With a broken finger, only a few milliliters of blood are lost, with a broken leg - 500-700 ml, with pelvic fractures - from 800 ml to 3 liters. If a vessel is damaged by a sharp bone fragment, massive blood loss is also possible in cases where the integrity of a relatively small bone (for example, the humerus) is damaged. The loss of a significant volume of bcc during fractures is one of the reasons for the development of traumatic shock.
First aid consists of anesthesia and immobilization with a splint. For open fractures, apply a sterile bandage to the wound. The patient is taken to the emergency room or trauma department. To clarify the diagnosis, radiography of the damaged segment is prescribed. For open fractures, PSO is performed; otherwise, treatment tactics depend on the type and location of the injury. For intra-articular fractures accompanied by hemarthrosis, a joint puncture is performed. In case of traumatic shock, appropriate anti-shock measures are taken.
Bleeding from other injuries
TBI can be complicated by hidden bleeding and hematoma formation in the cranial cavity. At the same time, a fracture of the skull bones is not always observed, and patients in the first hours after the injury may feel satisfactory, which complicates the diagnosis. With closed rib fractures, damage to the pleura is sometimes observed, accompanied by internal bleeding and the formation of hemothorax. With blunt trauma to the abdominal cavity, bleeding from the damaged liver, spleen or hollow organs (stomach, intestines) is possible. Bleeding from parenchymal organs is especially dangerous due to the massive blood loss. Such injuries are characterized by the rapid development of shock; without immediate qualified assistance, death usually occurs.
In case of injuries to the lumbar region, a bruise or rupture of the kidney is possible. In the first case, the blood loss is insignificant; bleeding is evidenced by the appearance of blood in the urine; in the second case, there is a picture of rapidly increasing blood loss, accompanied by pain in the lumbar region. With bruises in the lower abdomen, rupture of the urethra and bladder may occur.
First aid for all internal bleeding of a traumatic nature consists of pain relief, ensuring rest and immediate delivery of the patient to a specialized medical facility. institution. The patient is placed in a horizontal position with legs elevated. Apply cold (a bubble or heating pad with ice or cold water) to the area of suspected bleeding. If esophageal or gastric bleeding is suspected, the patient is not allowed to eat or drink.
At the prehospital stage, if possible, anti-shock measures are carried out and blood volume is replenished. Upon admission to medical school. the institution continues infusion therapy. The list of diagnostic measures depends on the nature of the injury. In case of TBI, a consultation with a neurosurgeon, skull X-ray and EchoEG are prescribed, in case of hemothorax - a chest X-ray, in case of blunt abdominal trauma - a consultation with a surgeon and diagnostic laparoscopy, etc.
Treatment in most cases is surgical - opening the corresponding cavity, followed by ligation of the vessel, suturing, and removal of the entire damaged organ or part of it. For minor bleeding, expectant management can be used, combined with conservative measures. For hemothorax, treatment is usually conservative - pleural puncture or drainage of the pleural cavity. In all cases, the patient’s condition is monitored and, if necessary, blood loss is compensated.
Non-traumatic bleeding
Non-traumatic bleeding from complete organs of the digestive system is quite common, mainly from the upper (esophagus, stomach), and less commonly, the lower parts of the gastrointestinal tract. The cause of esophageal and gastric bleeding can be Mallory-Weiss syndrome, erosive gastritis, peptic ulcer, malignant tumor, polyps and varicose veins of the esophagus with cirrhosis of the liver. Bleeding from the lower digestive tract can be observed with diverticula of the colon and small intestine, polyps, malignant tumors, Crohn's disease, ulcerative colitis, thrombosis or embolism of the mesenteric vessels, as well as ruptured aneurysms of the mesenteric arteries.
The diagnosis is made based on local (characteristic dark vomiting, melena) and general signs of internal bleeding. To clarify the source, special examinations are prescribed: FGDS, colonoscopy, etc. Treatment includes replenishment of the blood volume and elimination of the source of blood loss. For Mallory-Weiss syndrome, antacids, cold, aminocaproic acid and clotting stimulants are used; in severe cases, a gastrotomy is performed and tears in the mucous membrane are stitched. In case of peptic ulcer, tactics are determined by the rate of blood loss and FGDS data. In mild cases, endoscopic techniques (needling, electrocoagulation) are used; in severe cases, gastric resection is performed. For varicose veins of the esophagus, conservative treatment is carried out: a Blackmore probe is inserted and drug therapy is prescribed. If bleeding continues, an emergency laparotomy is performed with suturing of the subcardial part of the stomach.
Bleeding from the lungs and bronchi can develop with malignant tumors, severe forms of pulmonary tuberculosis, mitral heart defects, aortic aneurysm, bronchial foreign bodies, lung gangrene, pulmonary infarction, bronchial adenoma and bronchiectasis. The diagnosis is established on the basis of characteristic signs and data from additional studies: chest radiography, chest CT, bronchoscopy and angiography of the bronchial arteries. Depending on the cause of bleeding, both conservative and surgical treatment are possible. In some cases, endoscopic bronchial tamponade is performed.
Medicines
Photo: poddavleniem.ru
In case of gastric bleeding, the following conservative measures can be taken:
- Infusion therapy. To restore an adequate volume of circulating blood, crystalline and colloidal solutions are recommended.
- Blood replacement therapy. Indicated for severe blood loss and signs of hemorrhagic shock. For transfusion, erythrocyte and platelet mass, fresh frozen plasma, and cryoprecipitate are used.
- Antisecretory agents. They are represented by two groups of blockers - proton pumps and histamine H2 receptors. Medicines reduce the production of gastric juice and are not used at the same time.
- Fibrinolysis inhibitors. They have a hemostatic effect by stopping fibrinolysis. They inhibit the work of enzymes or the formation of coagulation factors (plasmin).
Before transfusion of blood components, a conversation is held between the attending physician and the patient and/or his relatives to warn about contraindications, possible complications of blood transfusion and the consequences of refusal. The procedure is not recommended for myocardial infarction, pulmonary edema, stroke, endocarditis, thromboembolism, valve defects, tuberculosis, rheumatism, severe kidney and liver diseases. In cases of massive blood loss, there are no contraindications for blood transfusion.
Prevention of relapse
After stopping the bleeding, relapse is prevented. Antisecretory drugs continue to be taken as prescribed by the doctor. If possible, the factors that caused blood loss should be eliminated. For example, conduct a course of eradication of Helicobacter pylori, which is a common cause of stomach and duodenal ulcers. To prevent bleeding from esophageal varices, beta2-blockers (propranolol) are prescribed.
Folk remedies
Photo: oprostatite.info
If gastric bleeding develops, traditional methods cannot be used. In the absence of timely specialized care, this condition can lead to the development of hemorrhagic shock and death of the patient. It is necessary to immediately call an ambulance and not self-medicate. During the period of remission, the following remedies can be used:
- 1 tbsp. l. horsetail is steamed for an hour in 250 ml of boiling water. The broth is filtered and consumed half a glass each time after meals.
- A tablespoon of pink immortelle flowers is infused in 250 ml of boiling water. Then the infusion is filtered and given to the patient 1 tbsp. l. every 2 hours.
- A decoction of blueberries is brewed and drunk like tea three times a day.
Parsley helps prevent stomach bleeding. In addition, decoctions of chamomile, bearberry, and yarrow are used. All these herbs have hemostatic properties. Any folk remedies are allowed to be used only after the approval of a specialist.
The information is for reference only and is not a guide to action. Do not self-medicate. At the first symptoms of the disease, consult a doctor.