The duodenum begins the human intestine - it is located immediately behind the stomach and is relatively small in size compared to other parts of this organ (see photo above). Also called DPC for short.
Why was it called that: Medieval scientists - anatomists did not have modern means of measurement, and after measuring the length of this organ with their fingers, they received an indicator of 12 fingers in diameter - 25 - 30 cm.
Functions of the duodenum
The duodenum plays an important role in the entire digestive process. Since it is the initial link of the intestine, the processes of absorption of nutrients from incoming food and liquid actively occur here. It brings the acid-base indicator of food to a level that will be optimal for subsequent stages of digestion in the intestines. It is in this organ that the stage of intestinal digestion begins.
Another integral phase of the work of this part of the intestine is the regulation of pancreatic enzymes secreted by the pancreas, as well as bile, depending on the acidity of the food bolus and its chemical composition.
The duodenum affects the proper functioning of the secretory function of the stomach, since the opposite interaction occurs. It involves the opening and closing of the pylorus of the stomach and humoral secretion.
Evacuation and motor functions.
The 12 duodenum carries the function of further promoting food gruel, treated with enzymes, into the next section of the small intestine. This occurs due to the massive muscle layer of the duodenal wall.
Duodenal diverticulum simulating a pancreatic cyst
Ultrasound machine HM70A
Expert class at an affordable price.
Monocrystal sensors, full-screen display mode, elastography, 3D/4D in a laptop case. Flexible transformation into a stationary scanner with a cart.
Introduction
A diverticulum (from Latin diverto, divertere - to fold, to direct in the other direction) is a protrusion of the wall of a hollow organ that communicates with its lumen. There are true and false diverticula, the former are rare, mostly congenital, single. Their wall has the same structure as a hollow organ (hence the name). Having a muscle layer, true diverticula are able to actively empty themselves, and their inflammation rarely occurs [2]. False diverticula are relatively common and represent a protrusion of the mucous membrane between the muscle fibers; their wall does not contain a muscle layer and they cannot actively empty themselves. This favors stagnation of contents and the development of diverticulitis.
Diverticula occur in weak areas of the wall, most often in tunnels formed by vessels that penetrate the muscle layer. Proximity to blood vessels creates a high risk of bleeding [4, 7]. That is why the clinical significance of the disease lies in the possibility of developing complications, including life-threatening ones [2].
In the diagnosis of diverticula of the digestive tract (they can occur in any hollow organ, but, as statistics show, they are more common in the colon), the leading place is occupied by the x-ray method, since endoscopic examination is noticeably inferior in accuracy. Thus, esophagogastroduodenoscopy (EGDS) detects a disease, for example in the duodenum, in only 1/3 of the patients for whom the diagnosis is established radiologically. For the stomach this figure is even lower [4].
In recent years, quite a lot of experience has been accumulated in ultrasound diagnostics of pathological conditions and diseases of the gastrointestinal tract [1, 3, 5, 6]. However, in the available literature we have not encountered a single case of successful ultrasound diagnosis of diverticula of the stomach or duodenum.
In this report we would like to share an observation that confirmed the possibility of echographic diagnosis of duodenal diverticulum.
Case description
Patient A., 66 years old, complained of short-term, periodically occurring aching pain in the epigastrium and right hypochondrium, not associated with food intake, a feeling of bitterness in the mouth, belching of air and food, heartburn, and nausea. From the anamnesis it is known that in 1982 a cholecystectomy was performed for cholelithiasis. Subsequently, I felt well, was not examined, and was not treated. The complaints described above have been bothering me for the last 4-5 weeks, and therefore I went to the doctor at the clinic at my place of residence, where an ultrasound of the abdominal organs revealed a pancreatic cyst.
Upon presentation: satisfactory condition, increased nutrition, skin and visible mucous membranes are clean, normal color. No abnormalities were detected from the cardiovascular system or lungs. Pulse 79 beats. in 1 minute, rhythmic, good filling. Blood pressure = 135/90 mm Hg. Art. The tongue is moist and covered with a gray coating. The abdomen is soft, moderately painful on palpation in the epigastrium. The liver is not enlarged and not palpable. Stool with tendency to constipation. There is no dysuria. Clinical and biochemical blood tests revealed no diagnostically significant deviations from the norm.
Ultrasound of the abdominal organs: the liver is not enlarged in size (4.3-13.3 cm), its contour is smooth, the parenchyma has moderately pronounced signs of fatty infiltration. No focal pathology was identified. The intrahepatic bile ducts and veins, portal (0.9 cm) and splenic (0.4 cm) veins are not dilated. The common bile duct is visualized in fragments, the diameter does not exceed 0.8 cm. The gallbladder is not visualized (surgically removed). The pancreas is of normal size (2.9-1.6-2.1 cm), the contour is smooth, evenly diffusely compacted. The duct of Wirsung is not dilated. The cross-sectional diameter of the digestive tract at the level of the esophageal opening of the diaphragm is 1.6 cm. There is a lot of mucus in the stomach on an empty stomach, its wall is not thickened (0.3-0.5 cm). At the level of the outer contour of the head of the pancreas, a rounded formation with smooth contours of reduced echogenicity is visualized with a delicate internal structure measuring 2.1 × 3.2 cm (Fig. 1). Polypositional examination failed to reveal the connection of this formation with the head of the gland. At the same time, locally, at the level of this formation, the thickness of the wall of the distal part of the duodenal bulb was 0.5 cm (in other parts 0.2-0.3 cm). The spleen is not enlarged, its structure is homogeneous. Free fluid in the abdominal cavity is not detected. The abdominal aorta is of normal diameter (1.8 cm). Para-aortic lymph nodes are not visualized. Conclusion: condition after cholecystectomy. Ultrasound signs of liver steatosis, hiatal hernia. Pancreatic head cyst? To exclude pathology of the stomach and duodenum, X-ray and endoscopic examinations are indicated.
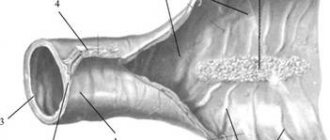
Rice. 1.
Echogram of a duodenal diverticulum simulating a pancreatic cyst.
X-ray of the stomach and duodenum: the act of swallowing is not impaired. The esophagus is freely passable; there is a significant size (up to 7 cm) hiatal hernia with severe reflux esophagitis and reflux of stomach contents into the distal esophagus, increasing in size when lying on the stomach. The stomach is usually located and contains mucus and fluid on an empty stomach. The folds of the mucous membrane are thickened, convoluted, and form serration along the posterior wall and greater curvature in the cardiac region. The pylorus is freely passable; prolapse of the gastric mucosa into the duodenal bulb is noted. In the descending branch of the duodenal loop, a pedunculated diverticulum measuring 3 cm with a large amount of mucus in it is detected (Fig. 2). The duodenal bulb is irritated, the barium suspension passes through it very quickly, and a reverse reflux of the barium mass into the stomach is noted. Conclusion: sliding hernia UNDER. Reflux esophagitis. Gastritis. Duodenitis. Duodenogastric reflux. Diverticulum of the duodenal loop with signs of diverticulitis. The patient categorically refused to undergo EGD.
Rice. 2.
X-ray of a duodenal loop diverticulum.
Conclusion
The duodenum is the most common location of small intestinal diverticula, which in 98% of cases are located on the inner wall of the duodenum, where they are embedded in the pancreatic tissue, and only in 2% - on the free outer wall [4]. Most often, diverticula are localized in the area of the major duodenal papilla; people over 40 years of age prevail. In approximately 30% of patients, duodenal diverticula are combined with other diseases: peptic ulcer, gastric polyposis, cholelithiasis, pancreatitis, colon diverticulosis. If patient conservative treatment does not produce the desired results, surgery is indicated.
The case under consideration is interesting in that a large duodenal diverticulum simulated a pancreatic cyst during ultrasound examination. Cysts (pseudocysts) of the pancreas are much more common than diverticula, so it is quite natural to conclude that the patient has a cyst. However, the absence of indications in the anamnesis for acute or chronic pancreatitis, an unsuccessful attempt to trace the connection of the identified fluid formation with the head of the pancreas during polypositional examination, and local thickening of the duodenal wall allowed us to suggest a possible other pathology and prescribe further examination.
Thus, when identifying a volumetric fluid formation of the pancreas (in the projection of the gland) during echography, it is necessary to include the pathology of the stomach and duodenum in the differential diagnostic search algorithm, not forgetting about diverticula, since, as S.V. rightly notes. Herman, “The key to early diagnosis of digestive tract diverticula is a high index of suspicion of the disease” [2].
Literature
- Burkov S.G. Ultrasound diagnosis of diseases of the gastrointestinal tract // Doctor. - 1997. - N 1. - P. 16-18.
- German S.V. Diverticular disease of the colon: myths and reality // Ros. and. Gastroenterology, hepatology, coloproctology. - 2000. - N 1. - P. 66-75.
- Clinical guide to ultrasound diagnostics / Ed. V.V. Mitkova. IV volume. - M.: Vidar, 1997. - 388 p.
- Krylov A.A., Zemlyanoy A.G., Mikhailovich V.A., Ivanov A.I. Emergency gastroenterology. Guide for doctors. - St. Petersburg: "Peter", 1997. - P. 139-164.
- Berstad A., Hausken T., Gilja OH Ultrasonography of the human stomach // Scand. J. Gastroent, 1996. - Vol. 220. Suppl. pp. 75-82.
- Gimondo P., Mirk P., Romano M., Jannetti G., Gallipoli A. Ecographia e tratto gastroenterico: Stato dell`arte // Giornale Italiano Di Ecografia. 2000. - Vol. 3.- N 2. S. 121-129.
- Telford GL, Appel D. Diverticulitis // Gastrointestinal emergencies / Ed. M. B. Taylor. 1997. - P. 571-576.
Ultrasound machine HM70A
Expert class at an affordable price.
Monocrystal sensors, full-screen display mode, elastography, 3D/4D in a laptop case. Flexible transformation into a stationary scanner with a cart.
Features of the structure of the organ (shape, location, fastening)
The shape of most people is varied, and even in one person, both the shape and the location of the duodenum can change over the course of a person’s life. It can be V-shaped, and resemble a horseshoe, loop and other shapes. In old age, or after weight loss, it is lowered compared to where the duodenum is located in young and middle-aged people and overweight people. But most often it originates at the level of the seventh thoracic or first lumbar vertebra, located from left to right. Then there is a bend with a descent to the third lumbar vertebra, another bend with an ascent parallel to the upper part and the intestine ends in the area of the second lumbar vertebra.
It is attached to the abdominal organs by connective fibers located on the walls. The upper part of the duodenum has the fewest such attachments, so it is mobile - it can move from side to side.
Diet
The patient will have to follow a special diet not only during the treatment period, but also after its completion to prevent relapses. The therapeutic diet is based on the principles of healthy eating and the exclusion of irritating foods.
What foods should you not eat if you have a peptic ulcer?
- spices and seasonings;
- marinades containing vinegar or acetic acid-based products;
- peeled tomatoes;
- raw fruits and vegetables;
- smoked meats;
- foods high in salt (salted fish, canned food, etc.);
- sausages and sausages;
- fried foods;
- alcohol (in any doses);
- carbonated drinks;
- mayonnaise and other fatty sauces (especially industrial ones);
- products containing harmful additives (monosodium glutamate);
- meat broths.
If you have a duodenal ulcer, frequent meals are necessary - the stomach should not be empty for more than 3 hours in a row (except for night sleep).
Duodenal ulcer is a disease that takes a long time and is difficult to treat. The therapy not always gives positive results, so you should take a responsible approach to your health: adjust your diet, give up bad habits, get more rest and avoid stress. Preventive measures will help maintain intestinal health and avoid dangerous complications of the disease.
For information about the causes, symptoms and treatment of ulcers, watch the video:
This article has been verified by a current qualified physician, Victoria Druzhikina, and can be considered a reliable source of information for site users.
Rate how helpful this article was
3.9 11 people voted, average rating 3.9
Did you like the article? Save it to your wall so you don’t lose it!
The most common diseases of the duodenum.
- Duodenitis is the most common ailment of the duodenum of acute or chronic type, manifested in the form of inflammation of the mucous membrane.
- Ulcer – develops as a result of chronic duodenitis. Chronic damage to the duodenum, in which ulcers form in the mucous layer.
- A cancerous tumor is a malignant neoplasm localized in different layers of the duodenal wall.
Duodenitis
More than 90% of patients develop chronic duodenitis. It can develop due to many factors, including:
- consumption of low-quality products;
- alcohol abuse;
- smoking;
- ingress of foreign bodies and toxic substances;
- other chronic intestinal diseases.
This disease manifests itself in the form of pain in the epigastrium of moderate intensity, weakness, belching, heartburn, nausea, turning into vomiting. Symptoms are often accompanied by fever.
A variation of this inflammatory phenomenon is bulbitis, in which the pathological process occurs only in the duodenal bulb. This form of duodenitis does not occur just like that - it is a consequence of other pathologies of the intestines or stomach. The cause of bulbitis can be:
- gastritis;
- stomach or duodenal ulcer.
If the disease is at an acute stage, the person feels pain and nausea and suffers from repeated vomiting. Acute bulbitis develops against the background of long-term use of a large group of drugs, or poisoning. In the chronic form, there is also an aching pain syndrome, sometimes it can be accompanied by nausea.
Patients also experience chronic duodenal obstruction, which occurs against the background of tumor processes, developmental anomalies and other disorders in the duodenum. It is expressed in a violation of motor and evacuation functions in this part of the intestine and is characterized by the following symptoms:
- heartburn;
- decreased appetite;
- feeling of heaviness and discomfort in the epigastric region;
- constipation;
- gurgling and bubbling.
The manifestation of this disease is influenced by the causes that caused duodenal obstruction, the stage of progression and how long ago the disease arose.
How does an ulcer form?
The bacteria Hilicobacter pylori, settling on the mucous membranes of the duodenum, secrete toxins that are products of their vital activity, as well as ammonia.
Ammonia compounds increase the secretion of hydrochloric acid, which begins to be produced in increased volume and corrodes the intestinal walls. This leads to the formation of damage that looks like erosion, but is characterized by deeper penetration.
If a person smokes or eats smoked or pickled foods, this further irritates the walls of the intestines and stomach, which become more vulnerable. An existing ulcer may increase in size, which will significantly worsen the patient’s condition and reduce the chances of recovery.