MALABSORPTION SYNDROME
(French mal disease + absorption; synonym:
malabsorption syndrome, impaired intestinal absorption syndrome
) - a clinical symptom complex caused by impaired absorption through the mucous membrane of the small intestine of one or more nutrients. The syndrome of impaired intestinal absorption can be primary (hereditarily caused) and secondary (acquired).
The absorption of monomers (monoglycerides, fatty acids, amino acids, monosaccharides) is preceded by hydrolysis (breakdown) of food polymers (proteins, fats, carbohydrates) under the influence of digestive enzymes. Violation of the breakdown of proteins, fats and carbohydrates due to insufficiency of digestive enzymes (digestive enzymes) is called digestive insufficiency syndrome (maldigestion). The combination of both types of disorders (splitting and absorption) was proposed to be designated as malassimilation. However, the tradition of M. s. has taken root in the literature. include malabsorption caused by both disorders of transport mechanisms and insufficiency of digestive enzymes.
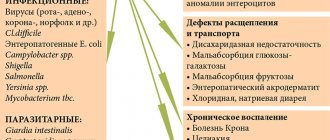
Etiology and pathogenesis
The direct cause of the disorder in the absorption of food ingredients may be the reduced activity of digestion enzymes and transport carriers of the final products of digestion through the intestinal wall. Another reason for M. s. is an insufficient supply of enzymes to the intestines with digestive juices due to blockage of the ducts of the glands of the mucous membrane of the small intestine with a viscous secretion, as is observed, for example, in cystic fibrosis. What matters is the lack of formation of enzymes that break down, for example, proteins, which leads to a deficiency of amino acids and protein starvation of the body.
Inactivation of cleavage enzymes and transport carriers also causes the development of M. s. Thus, some antibiotics (chlortetracycline, neomycin) can suppress lipid breakdown processes and increase steatorrhea (see).
When there is an excess of calcium and magnesium salts in food, fat absorption is impaired. In the emergence of M. s. Morphological changes in the small intestine and impaired peristalsis of the gastrointestinal tract are important. tract.
Pathogenetic mechanisms of M. s. diverse. With a deficiency of pancreatic enzymes, the cavity, or pancreatic, phase of digestion suffers; with a deficiency of intestinal enzymes (disaccharidases, peptidases, etc.), the surface, or membrane, phase of digestion is disrupted (see). Intestinal dysbiosis causes changes in the structure of bile cells, hepatobiliary diseases change their metabolism and are accompanied by cholestasis - all this contributes to the disruption of hydrolysis and transport of lipids (biliary phase). In various diseases and lesions of the small intestine, especially in the case of mucosal atrophy, the structures responsible for absorption processes (Cellular phase) are affected to varying degrees. In this case, the absorption epithelium transforms into glandular epithelium, and the diameter of the burrows on the surface of the mucous membrane through which absorption occurs decreases. A number of biochemical defects may occur: the number of transport carriers decreases, their structure changes, as a result of which their ability to interact with transported substances decreases; energy processes that ensure membrane transport are disrupted, etc. As a result of changes in the endocrine functions of the cells of the intestinal wall, the hormonal regulation of digestive and transport processes suffers. In case of disturbances in intestinal lymph flow and mesenteric circulation, further transport of absorbed substances (outflow phase) worsens. When the passage of food masses through the small intestine accelerates, due to motor disorders, the time of contact of chyme with the absorptive surface of the intestine is reduced.
3. Symptoms of malabsorption syndrome
The symptom complex in SMA usually combines a whole “bouquet” of disorders. Their set is closely related to the mechanism of development of the pathology that causes malabsorption syndrome. The most characteristic manifestations, expressed to one degree or another in any genesis of intestinal disorders, are dyspeptic in nature:
- stool disorders;
- vomiting and nausea;
- belching;
- flatulence;
- abdominal pain;
- decreased appetite.
The severity, frequency and severity of these disorders varies significantly and depends on age, medical history, concomitant diseases, heredity, and phenotype.
Quite often, malabsorption syndrome is combined with a variety of allergic manifestations. The most common allergy is to cow's milk protein.
Without proper treatment, SMA causes general somatic disorders:
- weight loss;
- dryness and cracks of the skin;
- anemia;
- hair loss and destruction of nail plates;
- weakness;
- decreased activity and performance;
- constant drowsiness;
- apathy.
Severe forms of malabsorption syndrome lead to functional disorders (for example, they can cause impotence, menstrual irregularities in women, convulsions).
About our clinic Chistye Prudy metro station Medintercom page!
Classification
There are several classifications of M. s. The following classification testifies to the multiplicity of etiological and pathogenetic factors underlying the occurrence of MS. 1. Primary M. s. (hereditarily determined): intolerance to disaccharides (lactose, sucrose, isomaltose, trehalose) - disaccharidase deficiency; peptidase deficiency (celiac disease); enterokinase deficiency; intolerance to monosaccharides (glucose, galactose, fructose); impaired absorption of amino acids (Hartnup disease, Cystinuria, tryptophan malabsorption, methionine malabsorption); impaired absorption of vitamins - cyanocobalamin (B12), folic acid. 2. Secondary M. s. (acquired): gastrogenic, observed after gastrectomy, with gastritis, stomach cancer; pancreatogenic, caused by various diseases of the pancreas (pancreatitis, cystic fibrosis, cancer, tumors of the islet apparatus, etc.); hepatogenic, observed in acute and chronic liver diseases, intra- and extrahepatic cholestasis; enterogenous, caused by various intestinal diseases (enterocolitis, celiac disease, Crohn's disease, diverticulitis, blind loop syndrome, infectious, parasitic, vascular intestinal diseases), as well as postoperative (resection of the small intestine); endocrine, observed in diabetes mellitus, hyper- and hypothyroidism; so-called Iatrogenic, caused by long-term use of antibiotics, laxatives, cytostatics and other drugs, as well as radiation therapy.
There are other classifications, for example, according to Polonovsky (C. Polonovski, J. Polonovski), the cut is based on the division of M. s. according to the type of its origin (impaired absorption of gastric and intestinal origin, due to bile deficiency, due to pathology of the pancreas).
With primary M. s. Most often, there is a selective deficiency of enzymes or transport carriers and, as a result, the absorption of one food substance or several substances similar in structure suffers.
With secondary M. s. Usually there is a deficiency of many enzymes and transporters, various mechanisms of malabsorption are realized, which leads to impaired absorption of a number of nutrients. Of the primary malabsorption disorders in adults, hl occurs. arr. intolerance to disaccharides (disaccharidase deficiency), mainly lactose, other forms of primary M. s. quite rare, most of them are observed in children. Secondary M. s., especially in an erased form, is relatively often noted in the clinic of gastroenterological diseases of adults.
Clinical picture
One of the most important wedge, symptoms of M. s. in children it is chronic, diarrhea, and a unique indicator of insufficient absorption is steatorrhea - increased excretion of lipids in feces. The child stops gaining weight, malnutrition develops, and then exhaustion, and growth retardation (hypostature) is observed. Depending on the duration and nature of the process, changes in other organs and systems increase: the skin becomes dry, with a pellagroid coloration; glossitis is pronounced, the tongue is red without papillae; swelling appears due to disturbances in protein and water-electrolyte metabolism; hypochromic anemia, hypokalemia, hyponatremia, hypocalcemia are noted. In some forms of M. s. changes in the urine are observed, for example, with milk intolerance associated with lactose deficiency; in some cases, lactosuria is noted in the urine (see). There may be seizures, osteoporosis or osteomalacia due to calcium deficiency in the body; bloating, intestinal colic due to hypokalemia and increased fermentation processes in the intestines. However, M. s. can proceed without any sharp disturbances from the gastrointestinal tract. tract.
In adults, wedge, picture of M. s. largely due to the nature of the underlying disease. The intensity of intestinal symptoms (stool upset, rumbling, etc.) depends on the degree of intestinal damage, on the involvement of the colon in the patol process, often there are no intestinal symptoms at all. General manifestations predominate, indicating violations of the basic metabolic processes and functions of a number of organs and systems, which is associated with insufficient supply of nutrients to organs and tissues.
Patients complain of increased fatigue, decreased performance, weakness, decreased appetite, weight loss, sometimes exhaustion up to cachexia (see). They experience dry skin, hair loss, and increased brittleness of nails. There may be diarrhea, steatorrhea, creatorrhea. In the blood - hypoproteinemia, dysproteinemia, changes in the composition of blood amino acids, in the urine - hyperaminoaciduria (see Aminoaciduria). The concentration of cholesterol, total lipids and their fractions in the blood serum decreases. Wedges and signs of thiamine deficiency (paresthesia in the limbs, pain in the legs, sleep disorders), riboflavin (cheilitis, angular stomatitis), nicotinic acid (glossitis, pellagroid skin changes), ascorbic acid (bleeding gums) and others are often observed vitamins (see Vitamin deficiency). A number of wedges, symptoms are caused by impaired electrolyte metabolism: hyponatremia (arterial hypotension, tachycardia, dry skin and tongue, thirst), hypokalemia (muscle weakness, muscle pain, weakened tendon reflexes, decreased intestinal motility, extrasystole, etc.), hypocalcemia (numbness of lips and fingers, increased neuromuscular excitability, osteoporosis), manganese deficiency (decreased sexual function). In severe cases, osteomalacia with bone fractures and tetany may occur. Iron deficiency and B12-folate deficiency anemia often occur. In the oral cavity there are atrophic processes, desquamative changes in the tongue, and sometimes periodontopathy. The skin becomes atrophic, dry, folded, acquires a dirty gray color, and pigmentation appears. Cracks appear around the mouth, eyes, and anus; in severe cases, the disease is complicated by eczema and neurodermatitis. Changes in the endocrine system are noted (hypocortisolism, sexual function disorders, etc.); in severe cases, pluriglandular insufficiency syndrome may develop with damage to the pituitary gland, adrenal glands, gonads, and thyroid gland (see Polyglandular insufficiency). Neurotic disorders and hypochondriacal conditions are often observed.
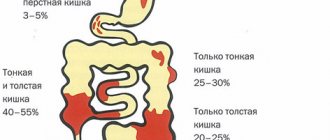
Klin, painting by M. s. to a certain extent depends on the localization patol. process in the small intestine. For example, when its proximal parts are predominantly affected, the absorption of calcium, iron, folic acid, and B vitamins is affected. When the middle parts are affected, the absorption of fatty acids and amino acids is impaired. Absorption of monosaccharides is impaired when the proximal and middle parts of the intestine are affected. When the distal parts of the small intestine are affected, there is insufficient absorption of vitamin B12 and bile cells, therefore, in the case of resection of the ileum, in some forms of Crohn's disease, the enterohepatic circulation of bile cells is disrupted.
With M., especially when the distal ileum is affected, the excretion of oxalates in the urine often increases - enteral oxaluria, which can lead to the formation of oxalate stones.
Malabsorption
Malabsorption, or, as it is also called, malabsorption syndrome, is a symptom complex caused by a disruption in the processes of absorption of nutrients, vitamins and microelements in the small intestine.
Malabsorption is often accompanied by insufficient digestion syndrome. Currently, under this name it is customary to combine more than seventy different pathologies affecting the digestive system.
Classification of malabsorption syndrome
Depending on the severity, malabsorption can be mild, moderately severe or severe:
- I degree of severity is considered the mildest and is characterized by a decrease in body weight (no more than 5-10 kilograms), decreased performance, increased weakness and the appearance of signs of general multivitamin deficiency;
- II degree of severity is characterized by severe body weight deficiency (in about half of the cases, weight decreases by more than 10 kilograms), pronounced symptoms of multivitamin deficiency, deficiency of electrolytes (calcium and potassium), symptoms of anemia, reduced function of the gonads;
- III degree of severity is characterized by a decrease in body weight by more than 10 kilograms in the vast majority of patients, severe symptoms of multivitamin deficiency (which are observed in all people in this group without exception), electrolyte deficiency, frequent seizures, manifestations of osteoporosis, the development of anemia, and the appearance of edema , dysfunction of the endocrine system.
Depending on the nature of the origin, malabsorption can be:
- Congenital;
- Acquired.
The congenital form occurs in only a tenth of all patients with malabsorption syndrome. As a rule, these are people who have been diagnosed with:
- Gluten enteropathy;
- Cystic fibrosis;
- Lactase deficiency;
- Sucrase deficiency;
- Cystinuria;
- Hartnup disease;
- Shwachman-Diamond syndrome, etc.
The acquired form of malabsorption is a consequence of:
- Transferred enteritis;
- Tropical sprue (a chronic, severe disease of the gastrointestinal tract of unknown etiology, which is characterized by pathological changes in the mucous membrane of the small intestine);
- Idiopathic hypoproteinemia;
- Chronic pancreatitis;
- Malignant neoplasms in the small intestine;
- Liver cirrhosis, etc.
Approximately three out of a hundred patients with acquired malabsorption syndrome have an intolerance to the protein contained in cow's milk.
This malabsorption syndrome is a hereditary pathology, as a result of which the absorption of monosaccharides in the stomach and intestines is disrupted.
This genetic disease is caused by a structural mutation of the gene responsible for the production of a transport protein in the body, which ensures the movement of glucose and galactose.
The main mechanism for the development of the clinical picture of glucose-galactose malabsorption is a violation of tissue respiration processes, resulting in:
- Red blood cells lose their ability to transport oxygen;
- Blood glucose levels are significantly reduced;
- The patient begins to show signs of mental and mental retardation.
Over time, galactose metabolites accumulate in the blood, which, accordingly, leads to an increase in their content in various tissues and organs and, as a consequence, to their damage. For example, glucose-galactose malabsorption in children can cause the development of cataracts or cirrhosis of the liver (again in childhood).
The first symptom of malabsorption in children, which is noted already in the first days of their life, is dyspeptic disorders, manifested by:
- Frequent loose (watery) stools with a specific sour odor;
- Signs of jaundice;
- Increased gas formation in the intestines;
- Colic;
- Vomiting;
- Increased liver size;
- Pain in the epigastric region;
- Poor appetite;
- Blood poisoning with E. coli.
Moreover, similar symptoms of malabsorption in children develop every time after products containing glucose and/or galactose enter their body. In particular, this applies to breast milk and artificial milk formulas.
Other symptoms of glucose and galactose malabsorption include:
- Mental and physical developmental retardation;
- Eating disorders manifested by severe underweight;
- Increased drowsiness;
- Dehydration of the body, as a result of which the child’s skin becomes dry and flabby;
- Acidosis;
- Decreased bone mineral density;
- Hemolytic anemia;
- Excretion of glucose in urine and feces;
- To whom.
Diagnosis
The diagnosis of malabsorption syndrome should be made as early as possible in order to avoid worsening metabolic changes and disruption of various organs and systems.
V. A. Tabolin, E. I. Shcherbatova, T. I. Korneva, V. P. Lebedev, E. K. Kurgasheva (1973) proposed a multi-stage system for clinical and biochemical diagnosis of intestinal malabsorption syndromes in children. The research begins with an assessment of anamnestic data and genealogical analysis (see Genealogical method). At the same time, pay attention to the presence of diseases in relatives. tract (gastritis, peptic ulcer, cholecystitis, enterocolitis, pancreatitis), respiratory system (chronic, bronchitis), metabolic disorders (diabetes mellitus, hyperthyroidism). Along with genealogical analysis, screening tests are envisaged, such as tests for various sugars in feces and urine; scatological examination, determination of stool pH, reaction of stool filtrate with trichloroacetic acid, boiling test. The following tests are used: Benedict's test for sugars, Welk's test for lactose and maltose, Helman's test for sucrose, determination of carbohydrate content in feces using Clinitest tablets using the Anderson method. These tests allow us to identify changes characteristic of individual syndromes.
If celiac disease is suspected (see), the greatest value is the study of the content of total protein, protein fractions, immunoglobulins, total lipids, cholesterol and phosphorus, potassium and sodium in the blood serum, rentgenol. research went.-kish. tract with a suspension of barium sulfate, radiography of long bones, as well as assessment of the effectiveness of the ongoing gluten-free elimination diet - exclusion from the diet of products from rye, wheat, barley and oatmeal (see Celiac disease).
To confirm the diagnosis of M. s. in case of cystic fibrosis (see), it is necessary, along with the determination of sodium and chlorine in sweat fluid, nail plates, and testing with DOX, to study the immune status, the functional state of the liver, as well as the proximal parts of the nephron.
In patients with exudative enteropathy (see Exudative enteropathy), muscle fibers are revealed during scatological examination; qualitative reactions indicate the presence of plasma proteins in the stool. With disaccharidase deficiency, a decrease in stool pH to 5.0 or lower is detected; extracellular starch is found in the coprogram; tests for sugar in urine and stool are positive. Of great importance in the diagnosis of disaccharide intolerance are stress tests with mono- and disaccharides (glucose, D-xylose, lactose, sucrose, etc.) followed by blood tests and their chromatographic identification in feces and urine, as well as the study of daily urinary excretion of carbohydrates and proteins.
If Hartnup's disease is suspected (see Hartnup's disease), along with the characteristic wedge symptoms, the determination of the content of indican, amino acids proline and argine in the urine is of great importance for the diagnosis. Positive tests of verification studies make it possible to conduct more in-depth studies using quantitative analytical methods: blood, daily urine, feces are examined; using an x-ray film test and a test with iodolipol, the activity of trypsin and lipase is assessed; identification of proteins in blood serum and feces is carried out. A study of the daily excretion of carbohydrates in urine reveals melituria (see) in the intestinal form of cystic fibrosis, disaccharidase deficiency, glucose and galactose intolerance. Identification of proteins in blood serum and feces using immunoelectrophoresis (see) makes it possible to diagnose exudative enteropathy. After conducting clinical biochem. By comparing the results obtained, the presumptive diagnosis is confirmed by targeted clinical, radiological and gastroduodenoscopic studies, which are carried out taking into account the data obtained earlier.
All of the listed methods are used in practice to establish the diagnosis of M. s. in adults. Methods for recognizing disorders of the absorption function of the small intestine - see Intestines.
Treatment
In case of primary (hereditarily caused) syndrome of intestinal malabsorption, an important component of complex therapy is treatment. nutrition, which provides for the limitation or exclusion of foods that lead to the development of patol, symptoms. Thus, in the treatment of celiac disease, the main thing is to use a gluten-free diet. A high-calorie diet with sufficient protein, vegetables, and fruits is prescribed; products made from rye, wheat, and oats are completely excluded.
In case of intolerance to disaccharides and monosaccharides, a diet with restrictions is necessary, and in some cases with the exclusion of those sugars that the patient cannot tolerate.
Treatment of lactose intolerance in infants is a difficult task, since in severe forms of deficiency it is necessary to exclude milk from the diet. In these cases, lactose-free milk formulas (galantamine, soyaval) are used. If there is a lack of sucrose, the child should not be transferred to mixed and artificial feeding early. Nutrition of children with intestinal and mixed forms of cystic fibrosis with a predominance of disorders from the gastrointestinal tract. tract, is based on compliance with the standards of products and menus accepted under normal conditions, but with a high content of proteins and carbohydrates, some limitation of fats, and a sufficient content of vitamins and mineral salts.
In case of intolerance to sucrose and isomaltose, sucrose is excluded and starch is limited; in case of intolerance to glucose and galactose, these monosaccharides are sharply limited, fructose is prescribed in increased quantities; in case of celiac enteropathy and other forms of severe enterocolitis, a gluten-free diet is recommended. In case of severe malabsorption of fats (for example, with cystic fibrosis), it is recommended to limit regular fats and prescribe triglycerides containing fatty acids obtained from coconut oil, which are easily hydrolyzed and absorbed in the intestines. In patients with severe forms of M. s. the so-called has a good therapeutic effect. nutritional diet, which is a mixture of amino acids, dextrin, trace elements, vitamins with the addition of small amounts of fat. This diet does not contain lactose, whole protein, is extremely low in waste and fat, and does not contain allergens.
Therapy for secondary (acquired) intestinal malabsorption syndrome involves treating the underlying disease. In severe cases M. s. Parenteral nutrition courses (glucose, protein hydrolysates, basic electrolytes, vitamins) are very effective. With M. s. due to intestinal dysbiosis, short courses of broad-spectrum antibiotics or eubiotics (8-hydroxyquinoline derivatives, Bactrim, etc.) are indicated; biol drugs (colibacterin, bificol, bifidumbacterin, etc.) are also recommended.
An essential role among to lay down. measures are played by means of replacement therapy. Preparations of pancreatic enzymes (Pancreatin, Panzinorm Forte, etc.), Abomin and a number of other enzyme preparations are prescribed; Only large dosages of these drugs are effective. The administration of enzyme preparations together with antacids, which significantly inhibit gastric secretion, helps to enhance the therapeutic effect of enzyme preparations for M. s. due to pancreatic insufficiency. Vitamins (A, D, K, C, folic acid, complex B, B12), calcium, magnesium, iron, cobalt are prescribed in pharmacodynamic doses. The administration of protein preparations (plasma, protein hydrolysates, protein, etc.) is indicated. With M. s. Cholestyramine is recommended due to dysfunction of the ileum (after its resection, in Crohn's disease, etc.), lignin (polyphepan) can be used for the same purpose, adsorbing unabsorbed bile cells and promoting their excretion in feces.
In cases of secondary M. s., caused by hl. arr. insufficient activity of membrane digestion enzymes, Difril (Corontin) in sufficient doses (at least 180 mg per day), as well as anabolic steroids (Nerobol, etc.), which stimulate the processes of membrane hydrolysis in the small intestine, are indicated. The phosphodiesterase inhibitor aminophylline and the inducer of lysosomal enzymes phenobarbital also increase the activity of membrane digestive enzymes. Some adrenomimetic drugs stimulate the absorption of monosaccharides in the small intestine - ephedrine, L-dopa, beta-blocker propranolol (obzidan, anaprilin), deoxycorticosterone acetate, aminophylline. The kinin inhibitor prodectin (parmidine), anticholinergic (atropine) and ganglion-blocking (benzohexonium) drugs have a normalizing effect on the absorption of monosaccharides - and at low initial rates they stimulate it, at high levels they inhibit it. For diseases where M. s. is secondary, when malabsorption is not associated with a deficiency of digestive enzymes or transport carriers, correction of intestinal absorption processes with the help of medications can be effective.
What is glucose-galactose malabsorption syndrome?
A pathology such as glucose-galactose malabsorption is a hereditarily determined syndrome caused by inadequate absorption of monosaccharides in the gastrointestinal tract. Often, together with a digestion disorder, the process of reabsorption of simple carbohydrates in the kidneys occurs.
What kind of syndrome is this
Glucose-galactose malabsorption syndrome is a rare genetic disease where the cells lining the intestines are unable to absorb galactose and glucose. The pathology is discovered after the birth of the baby. Adults also suffer from this disease.
A person with malabsorption constantly has problems digesting these sugars, because they are not able to be absorbed by the body. Because of this, the fluid ends up outside the body's cells, which leads to diarrhea and dehydration.
Glucose malabsorption leads to the appearance of sugar metabolites that accumulate in the kidneys and liver, which provokes dysfunction of these organs. A decrease in glucose levels creates active starvation of the cells of the central nervous system and other structures, as a result of which human development and growth are impaired.
Classification
Malabsorption syndrome has 3 degrees of severity:
- The first is the easiest, characterized by decreased performance, loss of body weight (5-10 kg), weakness, and insufficient amounts of vitamins and microelements.
- The second one has a significant decrease in weight, pronounced signs of multivitamin deficiency, a lack of potassium and calcium in the body, and anemia.
- The third – is expressed in a lack of electrolytes, osteoporosis, convulsions and swelling are possible, characterized by disruption of the functioning of the endocrine system.
Congenital type of malabsorption - found in 10% of all patients diagnosed with:
- cystic fibrosis;
- cystinuria;
- lack of sucrase;
- gluten enteropathy;
- galactosemia;
- Hartnup's pathologies;
- lactase deficiency and more.
Acquired syndrome occurs with the following illnesses:
- enteritis;
- cirrhosis of the liver;
- chronic pancreatitis;
- hypoproteinemia;
- with helminthic infestation;
- tumors located in the small intestine;
- autonomic neuropathy;
- colitis and more.
In some situations, the cause of the development of malabsorption syndrome is:
- osteoporosis;
- dysbacteriosis;
- increased intestinal motor function;
- hypovitaminosis;
- anemia.
Approximately 3 out of 100 patients with acquired glucose malabsorption syndrome have an intolerance to cow's milk.
Symptoms
The symptoms of malabsorption syndrome are so pronounced that a competent doctor can make a diagnosis during an examination or interview of the patient or parent.
Signs of the syndrome in adults and children include:
- constant diarrhea (up to 15 times a day), with an unpleasant odor, watery or pasty; stool is colorless and greasy;
- intense pain in the abdomen, concentrated in its upper zone, moving to the lumbar region. Possible rumbling, cramping or girdling pain symptoms;
- increased gas formation, colic;
- weight loss even with good nutrition;
- a person’s appearance changes – the skin is dull, dry, pigment spots appear, brittle nails, severe hair loss;
- Iron-deficiency anemia;
- fatigue – a person’s capacity is reduced, a constant feeling of weakness, powerlessness, drowsiness;
- signs of jaundice;
- vomiting, lack of appetite;
- development of cataracts;
- liver enlargement;
- coma.
In humans, secondary malabsorption is manifested by a clinical condition characteristic of the disease that caused its development.
Diagnostics
To identify glucose-galactose malabsorption syndrome, the following diagnostic methods are used:
- a careful study of the parents’ medical history, what the woman’s health was like during pregnancy;
- blood analysis;
- analysis of feces and urine (to determine glucose in them);
- breath test - performed to determine lactose intolerance.
Some clinical conditions have similar symptoms. Therefore, an additional specialist may prescribe x-rays, ultrasound, and endoscopy of the small intestine.
Therapeutic actions
After the appearance and diagnosis of glucose-galactose malabsorption, a person will need a certain diet (table No. 5).
Principles of nutrition for glucose-galactose syndrome:
- eat often;
- eat small meals (every 2-3 hours);
- the serving volume should be no more than 250 g;
- to replenish the supply of vitamins, you need to take foods with a high presence of vitamin C, B, folic acid;
- It is useful to eat various cereals, dietary lean meat, slightly dried bread, vegetables (beets, potatoes), fruits, berries (blackberries, bananas, raspberries), the basis of which is fructose in small quantities, cottage cheese with a small percentage of fat content, compotes, jelly;
- completely eliminate the intake of fatty meat, fish, smoked meats, marinades, mayonnaise, various seasonings, baked goods, semi-finished products, fast food, coffee, sorrel.
If a child has insufficient absorption of glucose-galactose, you need to be careful, especially during the first formula feedings, to watch the baby’s reaction. Completely remove products containing galactose, dairy products, and table sugar from the menu and replace them with fructose. In case of malabsorption syndrome, it is allowed to give mixtures containing different types of protein, purees.
Drug therapy
Having established the severity of the patient’s condition with malabsorption syndrome and its symptoms, the specialist can prescribe the following medications:
- parenteral – vitamins, microelements, protein mixtures are administered by injection;
- in order to eliminate dysbiosis, probiotics are used - products with live bacteria beneficial to the body, they help to establish intestinal microflora;
- enzymatic drugs;
- intestinal motility stimulants;
- immunomodulators;
- for intense pain, painkillers are used;
- medications that help the release and dilution of bile;
- More severe cases of malabsorption syndrome may require antibiotics.
Some major pathologies require surgical intervention:
- complex aggravation of intestinal inflammation;
- Crohn's disease;
- Hirschsprung's pathology.
Liver transplantation, colectomy, resection of lymph nodes, and sclerosis of the esophageal veins can be performed.
Prevention
Preventive measures for glucose-galactose malabsorption syndrome involve preventing illnesses that can cause its occurrence. These include:
- pathological changes in the pancreas, liver;
- inflammatory bowel diseases;
- endocrine system disorders;
- diseases of the gastrointestinal tract.
Prognosis and Prevention
Forecast for primary M. s. depends on the timeliness of the diagnosis and the correctness of the treatment; in case of secondary MS, it depends on the underlying disease and the effectiveness of the treatment.
Prevention of secondary M. s. consists of treating the underlying disease.
Bibliography:
Badalyan L. O., Tabolin V. A. and Veltishchev Yu. E. Hereditary diseases in children, p. 231, M., 1971; Vasilenko V. X. and Vinogradova M. A. About the problem of insufficient absorption of nutrients and the classification of its form, Klin, med., t. 45, No. 2, p. 9, 1967; Veltishchev Yu. E. et al. About intolerance to disaccharides in childhood, Vopr. ocher mat. and children, vol. 14, no. 12, p. 3, 1969, bibliogr.; G at b e r g r and c A. Ya. and L and Nevsky Yu. V. Diseases of the small intestine, M., 1975, bibliogr.; Complex therapy for diseases of the digestive system, ed. H. T. Larchenko and A. R. Zlatkina, M., 1977; Loginov A. S. et al. Treatment of patients with chronic diseases of the small intestine, Sov. med., No. 2, p. 63, 1979; Tabolin V. A. et al. Issues of diagnosis and treatment of malabsorption syndromes in children, Pediatrics, No. 3, p. 3, 1974; Physiology of absorption, ed. A. M. Ugoleva et al., L., 1977; F r about l-kiye A. V. Chronic enterocolitis, L., 1975, bibliogr.; Ament M. E. Malabsorption syndromes in infancy and childhood, J. Pediat., v. 81, p. 685, 1972; Bond JH a. L evitt MD Quantitative measurement of lactose absorption, Gastroenterology, v. 70, p. 1058, 1976; Gastrointestinal disease, ed. by M. H. Slei-senger a. J. S. Fordtran, p. 259, Philadelphia, 1973, bibliogr.; L osowsky MS, Walker BE a. K e 1 1 eher J. Malabsorption in clinical practice, Edinburgh, 1974, bibliogr.; Regan PT Konservative Therapie der Malabsorption, Leber Magen Darm, Bd 7, S. 201, 1977, Bibliogr.; Schreier K. Maldigestions-und Ma-labsorptionsyndrome, in the book: Klin. Gastroenterol., hrsg. v. L. Demling, Bd 1, S. 302, Stuttgart, 1973.
A. V. Frolkis; V. A. Tabolin (ped.).