Polyps in the intestines - is it dangerous? Symptoms and removal of polyps
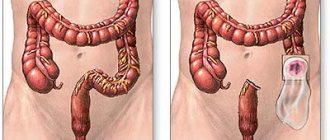
Polyps are benign formations that are localized on the mucous membrane and hang into the lumen. They are formed during a failure of epithelial regeneration, when new cells multiply at an abnormal speed and form growths that cover the intestinal walls with colonies, occupying a significant area.
As the epithelium grows, polyps can be damaged by feces, causing internal bleeding. Large growths can clog the lumen, contributing to constipation. Systematic damage to polyps can cause malignant formations, so the appearance of polyps is considered a precancerous condition and must be removed.
Causes
It is impossible to indicate the exact causes of polyps in the intestines. Experts only make assumptions by analyzing patient histories over the past decades. Doctors put forward several hypotheses that explain why polypous growths may appear on the intestinal walls. One of the main reasons is a chronic inflammatory process in the mucous membrane associated with poor nutrition, infectious diseases, bad habits, and low fiber content in the diet.
People at risk for polyp formation include people who:
- have undergone traumatic diagnostic or surgical procedures on the intestines;
- often consume drinks and foods that irritate the mucous membrane of the digestive tract;
- suffer from chronic constipation;
- engage in heavy physical labor;
- lead a sedentary lifestyle;
- eat fast food, fatty meats, fast food products that contain carcinogens and preservatives;
- abuse alcoholic beverages;
- have chronic gastrointestinal pathologies, especially of an infectious-inflammatory nature;
- get little fiber from food.
Formations with a high oncogenic risk appear due to the high content of animal fats and fried foods containing carcinogens in the diet. Due to the lack of fresh fruits and vegetables, intestinal motility decreases, its contents remain in contact with the intestinal walls for a long time. Carcinogens from processed food are absorbed into the epithelium, causing hyperplastic processes in glandular cells.
Causes of intestinal polyps
Reliable causes of the appearance of polyps (except for genetically determined syndromes) have not yet been established. It is assumed that the main risk factor is diet (as with colon cancer). A lack of dietary fiber (plant fiber) leads to retention of intestinal contents, which causes toxic digestive products to remain in contact with the mucous membrane for longer, disrupting its normal regeneration. The influence of concomitant diseases of the biliary tract cannot be excluded, in which the production of bile acids changes, which have a mutagenic effect on the mucous membrane. Chronic inflammation of various parts of the intestine is also important.
In addition, there are hereditary polyposis syndromes. They are transmitted in an autosomal dominant manner, i.e. from one parent to all children, manifesting itself in each generation.
Classification
Benign neoplasms in the intestine have different structure, shape, and size. There are also true polyps - growths of genetically altered mucosal cells and pseudopolyps, consisting of unchanged cells and appearing under adverse influences (for example, during a long-term local inflammatory process).
Polyps are classified according to their structure:
1) Glandular (adenomas). They consist of growing glandular tissue of the inner lining of the intestine, reach 2-3 cm in diameter, and are dense in consistency. Such formations are not prone to ulceration and bleeding. This type of polyp is more common and is more prone than others to degenerate into a cancerous tumor.
Varieties:
- tubular polyps, which are characterized by a pink color and a smooth surface.
- villous - medium-sized nodular or creeping along the wall of the formation, richly vascularized, therefore they are red in color and prone to bleeding, ulceration and necrotization;
- glandular-villous;
- tubular-villous.
2) Juvenile. Consist of embryonic tissues remaining in the intestinal wall due to developmental defects. Children under 10 years of age are most often affected, mostly boys.
3) Hyperplastic. These are small formations, up to 5 mm in size, soft in consistency, similar in color to the surrounding tissue. Hyperplastic intestinal polyp is rarely found in a single copy; more often the disease is multiple in nature.
4) Hamarthromas. Conglomerates of normal and altered epithelial tissue. They are thought to grow in the same way as surrounding tissue, but in a more disorganized manner. The incidence is associated with inheritance.
5) Lymphoid. It contains overgrown cells of lymphoid tissue. This type is often complicated by bleeding, and in a child it can cause intussusception.
Polyps occur in the form of:
- nodular formation of dense consistency;
- mushroom on a stalk;
- sponges with a lobed structure;
- bunch of grapes
By quantity they distinguish:
- single;
- multiple - up to hundreds, can be located in groups;
- diffuse - the number can reach several thousand.
The last two types are defined as intestinal polyposis; diffuse polyposis is inherited.
Diagnostic methods
Pathological formations in the rectum can be identified using a digital rectal examination. The proctologist performs this procedure during the appointment. To detect bleeding in the intestines, a stool occult blood test ( Gregersen test ) is performed.
The main method for diagnosing tumors in the colon is colonoscopy . During this examination, the doctor inserts a colonoscope - a special instrument in the form of a thin flexible tube with a video camera and a light source at the end. With its help, the intestinal mucosa is examined throughout. During a colonoscopy, you can perform a biopsy - obtain a sample of the changed tissue and send it to the laboratory for examination under a microscope.
Colonoscopy is the main screening method that helps detect the presence of polyps and colon cancer at an early stage. All people are recommended to have a screening colonoscopy after age 50. If a person has risk factors, for example, a family history, hereditary syndromes, inflammatory bowel diseases, he needs to start getting tested at an earlier age.
At the European Clinic, colonoscopy is performed by highly qualified expert doctors; we use modern generation diagnostic equipment from leading manufacturers. Our research is carried out in conditions that are comfortable for the patient, in a state of “medicated sleep”.
A so-called virtual colonoscopy may be prescribed. X-rays, CT or MRI are performed using contrast agents. These diagnostic methods are less accurate and informative compared to endoscopic examination of the intestine.
What is the probability of a polyp degenerating into intestinal cancer?
What polyps can develop into malignant ones? Almost 75% of all polyps in the intestine belong to these types of neoplasms; they are called adenomas or adenomatous polyps. According to the behavior of polyp cells under a microscope, in medicine it is customary to divide adenomas into subtypes - glandular-villous, villous and glandular (tubular). Tubular adenomas are least prone to malignancy, while villous adenomas very often lead to oncological degeneration.
The size of the formation also influences whether a polyp is at risk of malignancy. The higher it is, the higher the risk. When the growth exceeds 20 mm in volume, the threat worsens by 20%. Due to the fact that even the smallest polyps will steadily increase in size, they must be removed immediately after detection. There are also types of polyps that are not at risk of malignancy - these are hyperplastic, inflammatory and hamartoma formations.
- After eliminating the adenomatous formation, a person is advised to undergo regular examination to identify new polyps in the intestines;
- Large polyps are more likely to develop malignantly.
- Adenomatous formations are the most dangerous. They have a high potential for malignancy.
- Modern medicine has special tests that make it possible to diagnose hereditary predisposition to the development of intestinal cancer. This technique makes it possible to timely prevent the onset of oncological degeneration of polyps.
- Colonoscopy, sigmoidoscopy and sigmoidoscopy are diagnostic procedures that are mandatory for people over 50 years of age who have a dangerous heredity. If growths are not detected, then the next time you come to the clinic is recommended in two years.
Treatment of intestinal polyps abroad
The most effective way to remove intestinal polyps is surgery. The desire to cure a tumor formation at home will not bring the desired results, but will only aggravate the situation, since the pathology can go into a malignant stage, and valuable time will be lost.
Nowadays, to remove polyps, they resort to a treatment method such as TAMIS (transanal minimally invasive surgery). Previously, it was first tested in cancer centers in Israel, but now high-tech equipment and qualified doctors allow this procedure to be performed quickly and painlessly in leading clinics in post-Soviet countries.
In some cases, a combined surgical intervention is used: excision of a tumor formation and electrocoagulation of small polyps. Foreign surgeons perform polypectomy on an outpatient basis using a proctoscope and an elastic ligature. In their opinion, this method is quite simple, low-traumatic, and occurs without side complications when removing even large polyps.
If malignant degeneration of a tumor-like formation in the intestine is suspected, resection of the membrane surrounding the polyp is performed. Next, the doctor sends these removed tissues for histological and cytological tests to confirm the diagnosis. This approach is actively used in the treatment of cancer in Israel and other countries.
Symptoms
At the initial stage, polyps do not cause any symptoms, as they are small and few in number. Moreover, such neoplasms are difficult to detect using conservative research methods other than colonoscopy. With the further growth of non-malignant tumors, there is a risk of injury to them by flows of feces.
In this case, damage to the integrity of the polyp leads to the release of blood or mucus. Usually the bleeding is minor and is therefore only detected through occult blood tests. Any pain syndrome at this time is absent or so mildly expressed that it does not suggest the development of polyposis.
The presence of large polyps in the large and small intestines, on the contrary, can be diagnosed based on the existing symptoms. The patient has:
- Regular constipation. Feces pass on their own, but rarely and painfully, or with the help of enemas or laxatives.
- Bleeding from the anus. Patients often confuse this symptom with anal fissures, hemorrhoids and fistula. As a rule, bleeding is accompanied by a large amount of mucus.
- Foreign body sensation. The feeling occurs in the rectum near the anus.
- Painful sensations. Large polyps cause cramping pain in the intestinal area (in some cases confused with flatulence). Painful sensations may also appear in the lower abdomen.
- Damage. Constipation causes an inflammatory process where solid stool damages the intestinal walls. Anal fissures often appear, which must be treated with antiseptics and anti-inflammatory drugs. If this is not done, purulent fistulas may form.
- Diarrhea. Frequent bowel movements with loose stools. Blood, pus, and serous discharge may be present.
- Dropping out. If the tumor is located in the rectum, it may fall out during defecation, or block the passage of feces near the sphincter. This symptom is also accompanied by bleeding.
- Exhaustion. Polyps are soft tissue that grows due to nutrition. It enters through the circulatory system and lymphatic currents. The patient often experiences an increase in appetite, or, conversely, a decrease. Symptoms of anemia may be present: pale skin, circles under the eyes, dizziness, nausea, headaches. In some cases, anemia is a clinical symptom.
A coloproctologist examines and prescribes treatment. The main method for detecting polyps is colonoscopy.
Diagnosis of polyps in NEARMEDIC
Regular stool examination can detect traces of hidden blood. This does not necessarily indicate the presence of growths, but it is a symptom that requires additional health care. However, you should not limit yourself to tests, since the absence of blood does not indicate the absence of polyposis.
What studies diagnose the presence of formations:
- CT and MRI of internal organs;
- sigmoidoscopy to examine the intestinal walls;
- flexible sigmoidoscopy;
- irrigoscopy detects growths from 1 cm;
- the most informative technique is colonoscopy (with collection of biomaterial in the presence of a polyp).
A histological and cytological examination of the biopsy is carried out to identify the type of formation.
Polyps in the intestines - treatment or removal?
There is no conservative, drug treatment for intestinal polyps. Sometimes, during rectal endoscopy, it is possible to remove polyps in the intestine if they are small in size and well located. In other cases, surgery is required. If the polyp is located low in the rectum, it can be removed transanally.
If small polyps are detected during colonoscopy, during the endoscopic procedure they can be removed using a loop electrode, by electrical excision, when the stalk of the tumor is clamped with an electrode. In some cases, polypectomy can cause perforation of the intestinal wall and be complicated by bleeding. In all cases, removed intestinal polyps are examined histologically. If the histology results give a positive conclusion about the presence of cancer cells, they resort to resection of this section of the intestine.
The following types of surgical intervention are distinguished:
- Electrocoagulation. The procedure is performed by inserting an operating colonoscope through the anus. Through this instrument, a special loop is inserted into the intestinal lumen, which passes a current, causing it to heat up to a certain temperature. She grabs the polyp and cuts it off.
- Transanal excision. This type of surgical intervention is recommended for patients with pathological formations located no deeper than 10 centimeters from the anus. During the operation, local anesthesia is used. Then the anal canal is expanded using a special speculum and the polyp is excised with scissors or a scalpel, after which sutures are placed on the mucous membrane.
- Transanal resection of the rectum. It is recommended for people with precancerous lesions. Its essence is to remove the rectum through the anus and remove the affected area along with the formations.
- Transanal endomicrosurgical excision. The operation is performed through the anus using a rectoscope. An endoscopic loop is inserted through the instrument and the formation is cut off. The procedure is most often used to remove large villous polyps.
- Colotomy. This is a surgical procedure performed through an incision in the abdominal cavity. A certain intestine is pulled out through the wound, followed by removal of the formations. This procedure is performed when transanal interventions using a proctoscope and other instruments are difficult.
For familial, diffuse polyposis, and especially when it is combined with tumors of other tissues or Gardner's syndrome, treatment involves complete resection of the large intestine, with the anus connected to the end of the ileum. 1-3 years after removal of large polyps, relapses of the pathology may occur, so it is recommended to perform a colonoscopy one year after the operation and perform endoscopic diagnostics every 5 years. Large and multiple polyps, as well as familial polyposis, have the greatest risk of degeneration into cancer.
To date, there are no preventive measures that can prevent the development of polyps in the intestines. Therefore, only timely regular diagnosis after 40 years or with a genetic predisposition to intestinal cancer can determine the presence of oncogenic polyps in the body in the early stages of their development. With timely detection and removal of cancer cells, recovery occurs in 90% of cases.
Types of benign intestinal tumor formations and their symptoms
Typically, a polypous formation inside the intestine is benign, forming from epithelial tissue cells and growing into the intestinal lumen. Polyps vary in size, shape, they can “stand” on a stalk or on a broad base, single, multiple (polyposis), soft texture.
Intestinal pathology in the form of polyps is usually observed in older people, overweight people, diabetics, and heavy smokers; it can also be caused by genetic mutations.
Considering the frequency of occurrence of polyps in different parts of the intestine, you can notice that most of them develop in the sections of the colon and rectum, and less in the small intestine. In the duodenum, polyps are diagnosed quite rarely (approximately 0.2% of all endoscopic examinations).
A tumor-like growth in the form of a polyp is not oncology, but over time there is a possibility of its transformation into a malignant tumor.
There are many types of polypous formations in the intestines, but among them the most common are:
- Adenomatous , which are observed in approximately 70% of older patients. It is this type of tumor formation that is more likely than others to degenerate into a low-quality tumor.
- Serrated polyps, depending on their size and location, have varying degrees of malignancy. If small formations are located in the lower region of the colon, the risk is minimal, but if the polyp is large and located in the upper region of the intestine, then the risk of malignant transformation increases.
- Inflammatory polyps are formed when intestinal pathologies such as Crohn's disease and ulcerative colitis occur. Although this type of tumor-like growth has a low percentage of degeneration into oncology, the treatment process should not be neglected.
The effectiveness of treatment of intestinal polyps abroad depends on an accurate diagnosis and determination of the type of pathology.
Nutrition rules
The diet of patients who have undergone surgery to eliminate polyps in the intestines should be gentle and include at least six meals a day. The foods you eat should contain a large amount of plant fiber, antioxidants and vitamins.
Contraindicated for use:
- milk products;
- any canned food;
- pickles;
- smoked meats;
- fried and fatty foods;
- refined products containing large amounts of flavors and dyes.
Benefits for the patient:
- sea and white cabbage;
- pumpkin dishes;
- fresh carrots, onions, spinach;
- wheat sprouts;
- pureed soups and cereals;
- all types of fermented milk products;
- green tea;
- fruits of non-acidic varieties;
- lean meats, boiled or steamed.
All food should be warm (excessively cold and hot dishes are harmful to the patient). Protein foods should not be consumed together with starchy foods.
Folk remedies
Treatment with folk remedies has no scientific basis and does not bring the desired result to patients who refuse tumor removal.
There is a lot of information on the Internet about the use of celandine, chaga, St. John's wort and even horseradish with honey, which can be taken orally or as enemas. It is worth remembering that such self-medication is dangerous not only in terms of wasting time, but also injuring the intestinal mucosa, which leads to bleeding and significantly increases the risk of malignancy of the polyp.
Prognosis and prevention of intestinal polyps
Adenomatous polyps sooner or later degenerate into a malignant tumor, so they must be removed routinely.
There is no specific prevention of polyps. Proper nutrition, giving up bad habits, and timely treatment of inflammatory bowel diseases will help reduce the likelihood of their occurrence.
1 A.O. Shalaurov, I.I. Romanova, L.V. Shalaurova. On the issue of treatment and prevention of intestinal polyposis. Biological medicine, 2008.
2 V.I. Yukhtin. Polyps of the gastrointestinal tract. 2008.
3 Lapteva E.A., Kozlova I.V., Myalina Yu.N. et al. Colon polyps: epidemiology, risk factors, diagnostic criteria, management tactics (review) // Saratov Journal of Medical Scientific Research. 2013.
Prevention
In order to reduce the risk of developing polyps in the intestines, you should adhere to certain preventive rules, which include:
- to give up smoking;
- active lifestyle;
- timely and complete treatment of intestinal diseases;
- proper nutrition;
- eliminating constipation;
- giving up alcohol;
- preventive examination of the intestines once every 3 years, and more often if necessary.
If a person is at risk for the formation of polyps in the intestines, he should consult with a doctor in advance, select an individual scheme for preventive examinations of the intestines and find out exactly about the very first symptoms of polyps that he may experience. These actions will either prevent the disease, or, if it occurs, help to successfully cope with it.
Symptoms of pathology
In most cases, a person who has polyps in the rectum or colon does not experience direct signs of pathology. For this reason, the disease is detected already in an advanced form or when complications arise. Any dysfunction of the gastrointestinal tract is a reason to consult a doctor and undergo a full examination.
With polyposis, patients experience defecation disorders, blood and mucus may be present in the stool, abdominal pain, nausea, discomfort, and frequent urge to defecate.