Definition
The term "diverticular disease of the colon" (synonymous with diverticulosis of the colon) is a sequence of anatomical and pathophysiological changes associated with the presence of diverticula (a sac or reservoir in the wall of any hollow organ - in this case, the intestine). These changes most often occur in the sigmoid colon, but can also affect the entire colon. This sequence can vary from the presence of a single diverticulum to multiple diverticula (which may be difficult to count).
Causes of diverticula
The occurrence of this disease does not have any specific cause. It is caused by a combination of many factors. There is an opinion that some people are predisposed to this disease due to congenital underdevelopment of the muscular layer of the intestinal wall. As a result, diverticula form with age or under the influence of any factors.
Congenital predisposition plays a role in people with hereditary syndromes of connective tissue dysplasia (Marfan syndrome, Ehlers-Danlos syndrome, when there is a deficiency of collagen in the human body), and a combination of diverticular disease of the colon with diseases associated with a decrease in the elasticity and strength of connective tissue (hernias) is also often found , varicose veins, visceroptosis, polycystic disease). However, congenital tissue deficiency is not the only cause of pathological changes in the intestinal wall.
The high incidence of diverticular disease in older people is associated with a gradual decrease in the tone of the colon wall as the body ages. Diverticular disease is a chronic disease that occurs due to the formation of a pouch-like protrusion (diverticulum) in the intestinal wall, and, as a consequence of the stagnant process, the development of inflammation in them. The muscle layer of the colon becomes thicker and less elastic. The supporting connective tissue loses elasticity and the intestinal wall becomes less extensible. Therefore, diverticula appear more often in older people than in younger people.
It is also known that diverticula occur significantly more often with a decrease in plant fibers and fiber in the diet. Therefore, diverticular disease occurs 3 times less often in vegetarians than in people who limit their intake of vegetables and fruits. Foods low in fiber do not stimulate intestinal motility well, the movement of contents through the colon slows down, which increases water absorption and, as a result, constipation develops. Retention of feces in the intestine, combined with disruption of the normal intestinal microflora, leads to inflammation and progression of diverticular disease. This can also explain the more frequent appearance of diverticula in the sigmoid colon (constipation plays the role of a resolving factor).
The clinical picture in approximately two out of three cases is not accompanied by any complaints (asymptomatic diverticulosis); the pathology is discovered by chance during endoscopic or x-ray examinations. Most often, the first signs of diverticular disease are pain and functional impairment in the form of constipation or diarrhea. There are complaints of regularly recurring pain in the abdomen, often in the left iliac region or lower sections, which disappear after defecation. Pain of varying intensity can exist for a long time - from several weeks to months. Increased pain is sometimes accompanied by an increase in temperature, and signs of intoxication may appear (dry mouth, nausea, tachycardia). Also often noted is bloating and excessive gases, various dyspeptic disorders, which are sometimes hidden under the guise of irritable bowel syndrome.
Epidemiology of diverticulosis
Since the beginning of the 20th century, there has been an increase in the incidence of colonic diverticulosis in industrialized countries. The incidence of this disease increased with age and a diet high in red meat and refined sugar but low in whole grains, fruits and vegetables. It has been established that the risk of developing diverticular disease reaches 5% at the age of 40 years and can rise to 80% by the age of 80 years. The incidence of acute diverticulitis increases proportionally. As a rule, from 10 to 20% of patients with diverticulosis experience acute diverticulitis. Of those who require hospitalization, 20 to 50% of patients require surgical treatment.
Women experience complications of diverticulosis requiring surgical correction on average 5 years later than men. Men are more likely to bleed than women, but women have a higher incidence of diverticulum fistula formation. Younger men are more likely to get fistulas than older men. Bleeding is more common in older people.
Treatment of intestinal diverticulosis
Since it is necessary to treat diverticulosis taking into account the causes of its occurrence, the patient must be prepared to change his lifestyle, first of all, to a significant change in his diet. A special diet is the basis for the treatment of this disease, regardless of its form, since the causes of divertriculus lie mainly in poor nutrition. Additionally, medications are used, and in difficult cases, surgery.
Diet
Diet forms the basis of treatment for uncomplicated and asymptomatic diverticulosis. It is recommended to include more fiber products in the diet of patients. They increase the volume of stool and help reduce pressure in the intestines, which promotes faster and easier bowel movements. Fiber prevents further progression of diverticula, and in some cases leads to their regression.
The menu includes the following sources of fiber:
- bran bread or wholemeal bread;
- cereal porridge (wheat and buckwheat) with the addition of vegetable oil;
- vegetable casseroles or vegetables baked on a wire rack as a side dish;
- soups with meat or chicken broth and vegetables;
- dairy products.
In addition to vegetables and fruits, it is useful to include wheat bran in the menu. This should be done gradually so as not to provoke intestinal irritation. The initial daily intake is from 5 to 10 g of bran, then it is increased to 30 g.
To prevent the bran from damaging the intestinal walls, it is recommended to pour boiling water over it for half an hour and drain. You can add steamed bran to vegetable dishes, cereals, yogurt and soups.
Pasta and baked goods, semolina and rice porridge, jelly, strong coffee and tea, wine (red), and cocoa products should be excluded from the diet.
Drug therapy
With colonic diverticulosis, symptoms and drug treatment are directly related. The list of medications that are recommended for patients with this diagnosis includes:
- antispasmodics - Mebeverine, No-Shpa, Meteospasmil, Bucopan - are often used at the initial stage of therapy;
- sources of dietary fiber - Mukofalk, Solgar, Ispagol - replace bran, as they do not cause flatulence and cramps, stimulate the restoration of intestinal microflora;
- probiotics - Linex and its analogues - to restore microflora;
- prebiotics for loosening stool based on lactulose - Duphalac, Normaze and others;
- enzyme preparations are prescribed for severe digestive disorders, as well as in the presence of an inflammatory process;
- stimulants of intestinal motility - Motilium, Motilak, Domperidone;
- Broad-spectrum antibiotics are prescribed for inflammation of diverticula.
If treatment with medications does not lead to improvement, the patient is hospitalized and given infusion therapy. At the same time, additional research is being carried out and the issue of surgical intervention is being considered.
Surgery
Surgical intervention is used if diverticulosis of the descending section (or any other) worsens more than 2 times. In such situations, it is important to prevent intestinal perforation and the development of peritonitis, which often occurs with repeated attacks. For patients over the age of 40 years, elective surgical intervention is prescribed after the first exacerbation.
Also indications for the operation are:
- intestinal bleeding;
- intestinal obstruction;
- intestinal perforation;
- suppuration of the diverticulum with threatening or ruptured abscess.
During surgery, part of the intestine affected by diverticula is removed; the volume of intervention is determined individually.
The prognosis for timely diagnosed disease is favorable. More than 80% of operations are completed without subsequent complications, the risk of relapse is no more than 25%.
Pathophysiology
Diverticulosis occurs due to increased intraluminal pressure in the colon. In patients with diverticular disease of the colon, the intraluminal pressure exceeds 90 mm. rt. Art. during peak contraction of its walls. This is 9 times higher than the norm in healthy subjects. Abnormally high pressure leads to segmentation of the intestine. Segmentation results in a process in which the colon functions as a group of individual segments rather than as a single tube. The high pressure created in each such section acts directly on the intestinal wall, and not in the direction necessary to move intestinal contents into the rectum. This pressure causes the mucosa to protrude through the muscular layers, which occurs in areas where vessels penetrate to nourish the submucosal layer and mucosa. Most of these vascular penetrations are located between the mesenteric and antimesenteric tena, where diverticula are identified, respectively. When the mucous membrane bulges, it does so without involving the muscularis propria and forms a diverticulum only from the mucosa. The area of high pressure most often coincides with the sigmoid colon, which is the main site of manifestation of the disease.
Clinical manifestations
The disease can be asymptomatic (diverticulosis) or complicated by inflammation (diverticulitis). Mild inflammation of the mucous membrane, caused by a violation of the microflora, can cause damage to the nervous system of the wall of the colon and thereby lead to dysfunction of the colon, which leads to the formation of symptoms of its diseases. This explanation of symptoms in irritable bowel syndrome can easily be extrapolated to patients with diverticular disease of the colon, since studies of the colonic microflora in some patients with diverticula have revealed bacterial overgrowth.
The following symptoms may appear: functional disturbances in the motor activity of the colon of varying degrees of severity, as well as inflammation of varying degrees (localized) or complicated with multiple interactions with surrounding tissues, manifested in diffuse peritonitis or septic shock. These more complex symptoms and associated complications arise from disruption of the integrity of the wall of one or more diverticula. Typically, these complications do not occur until microperforation of the colon wall overlying the diverticulum develops into the paracolic space (fiber around the colon). It has been established that perforation can cause the formation of a microabscess, phlegmon, large abscess, fistula, or even perforation into the free abdominal cavity. Perforation into the free abdominal cavity occurs rarely, whereas fistula formation is more common, with the bladder being the most common organ where this diverticulum fistula perforation occurs.
The true communication between the perforation cavity around the diverticulum and the lumen of the colon is usually quickly closed by inflammatory swelling of the tissue. Sometimes the inability to obliterate the neck of the diverticulum leads to free communication between the lumen of the colon and the free abdominal cavity with the formation of peritonitis. Rupture of an isolated diverticulum abscess can also lead to purulent peritonitis.
Diverticulitis and diverticulosis
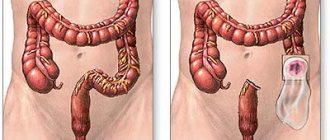
Quite often, patients confuse the diagnosis of diverticulitis and diverticulosis. Despite the fact that the diseases are similar to each other, it is worth distinguishing them, since treatment and diagnosis are different. A diverticulum is a growth that appears on the intestinal wall. It has a convex shape due to the fact that the layers of the intestine are deformed and stretched. The presence of one or many diverticula leads to a pathology called diverticulosis . In this case, there is no inflammatory process.
The inflammatory process of a diverticulum, accompanied by a number of symptoms, is called acute diverticulitis. It is worth distinguishing between these diseases, since diverticulitis of the small intestine will require surgical intervention. For diverticulosis, conservative treatment methods are sufficient.
Classification of diverticulitis
Acute diverticulitis
presents with signs and symptoms of acute inflammation and can be simple (limited to the intestinal wall and adjacent tissues) or complex (with perforation into the free abdominal cavity or with a fistula). Simple acute illness is usually accompanied by systemic signs such as fever and leukocytosis, while complex acute illness may have additional signs such as tachycardia and hypotension.
Complicated acute diverticulitis
can be classified according to the breadth of the inflammatory process. The general classification of diverticulitis with perforation was first described in 1963 by Huges and slightly modified and popularized by Hinchey in 1978. Stage 1 diverticulitis is a localized peri-intestinal or intra-mesenteric abscess. Stage 2 is limited to a pelvic abscess, stage 3 is generalized purulent peritonitis, stage 4 is generalized fecal peritonitis.
Diverticula of the large intestine.
Diverticula of the large intestine can be congenital (usually single), true or acquired (or pseudodiverticula).
Congenital diverticula are protrusions of all layers of the intestine and have a fairly wide entrance. Acquired diverticula are protrusions of the mucous-submucosal layers of the intestine through intermuscular gaps in the intestinal wall at the site of the passage of blood vessels.
One of the manifestations of diverticulosis can be intestinal bleeding, but in 80% of patients it is asymptomatic.
Most complaints from patients with colonic diverticulosis are related to irritable bowel syndrome. These are abdominal pains that intensify after the passage of gas and bowel movements. There may be flotulence (increased gas formation in the intestines), flatulence, and irregular bowel movements.
Upon examination, pain is revealed along the large intestine, abdominal bloating is noted, and a spasmodic, painful sigmoid colon is palpated.
With the development of complications of colon diverticulum, corresponding symptoms appear.
Complications of diverticulosis of the large intestine.
If there are several diverticula, this is already diverticulosis (diverticular disease). 80-95% of diverticula are located in the sigmoid colon.
inflammatory process – diverticulitis; if the inflammatory process is limited to the tissues surrounding the diverticulum, it is peridiverticulitis. As the latter progresses, the inflammatory process spreads to the underlying tissues, retroperitoneal tissue, and pericolitis develops. And the latter can be complicated by diverticulum perforation, abscessation, fistula formation and peritonitis. Diverticular disease of the large intestine affects 10% of people aged 30-40 years and 40% - 70 years and over.
In 20% of cases, colonic diverticulosis begins without symptoms, and only 5% of patients develop complications.
Diverticulitis -20%, it is promoted by chronic constipation, the formation of fecal stones in diverticula, which in turn can cause inflammation of only the diverticulum, if the intestines are not treated, the inflammation will spread to the surrounding tissues, mucous membranes, organs - peridiverticulitis.
If inflammation spreads to the entire intestinal wall and mucous organs, this is pericolitis, which can lead to perforation.
The latter is complicated by the formation of an abscess, the development of peritonitis and the formation of fistulas.
Widespread recurrent diverticulitis can lead to scarring of the intestine and cause obstruction - ileus.
Symptoms of acute diverticulitis.
Colicky abdominal pain, high body temperature, inflammatory changes in blood tests, poor general health, weakness. There may be diarrhea or constipation, vomiting, and loss of appetite. When the bladder and ureters are involved in the inflammatory process, dysuria, hematuria and pain in the kidney area, respectively.
Upon examination, abdominal bloating, painful palpation, and painful, spasmodic areas of the large intestine are revealed. Defense of the abdominal muscles indicates the presence of peritonitis.
Bleeding from diverticula.
Most often, the source of bleeding is in the sigmoid, cecum, descending colon. These bleedings, after angiodysplasia, rank second among the causes of bleeding from the anus.
Diverticulum perforation.
Sometimes peridiverticulitis is complicated by closed perforation, which can be asymptomatic or accompanied by local peritonitis. Perforation of a diverticulum can result in an abscess or various fistulas. Sometimes there may be purulent peritonitis without perforation of the diverticulum - contact.
Open perforation of a diverticulum into the abdominal cavity is uncommon.
Perforation of a diverticulum into the free abdominal cavity is an open perforation followed by purulent peritonitis. The mortality rate for this condition is about 50%.
Intestinal stenosis.
The sigmoid colon is most often affected, clinically this is manifested by episodes of partial intestinal obstruction.
Fistula formation.
In this case, fistulas can form between individual loops of the intestine, between the intestine and the genitourinary system, between the intestine and the skin. The incidence of this diverticulum complication is about 10%.
Manifestations of intestinal-vesical fistulas can be recurrent infections of the genitourinary system, excretion of gases and feces in the urine.
Diagnostics.
Uncomplicated diverticulosis of the large intestine is often detected incidentally during irrigoscopy or colonoscopy. Diverticulum is characterized by: abdominal pain, which usually occurs acutely, fever, changes in blood tests - increased leukocytosis, stab shift to the left, accelerated ESR, changes in the intestines detected during fibrocolonoscopy and irrigoscopy. With irrigoscopy (graphy) with double contrast, diverticula look like limited contrasted protrusions of the intestinal wall, in the form of round or oval formations with contrast.
With diverticulitis, deformation of the diverticulum, narrowing of the neck of the diverticulum, the presence of incomplete diverticula, irregularity of mucosal folds with preserved contractions or segmental haustration.
With fibrocolonoscopy, diverticula are clearly visible when the colonoscope is inserted and worse when it is removed. With diverticulitis, you can see swelling and redness of the mouth of the neck of the diverticulum. In acute diverticulitis, there is an increased risk of perforation during intestinal fibrocolonoscopy. CT and ultrasound can provide some information regarding complications of diverticulum.
In order to prevent diverticulosis of the large intestine and prevent its complications, it is recommended: timely treatment of chronic constipation, irritable bowel syndrome (IBS). This is achieved by taking a sufficient amount of liquid, avoiding overload of the cardiovascular system (1.5-2.5 liters), a diet rich in dietary fiber (vegetables, fruits, bran), excluding spicy and irritating foods to the gastrointestinal tract.
Helps normalize stool:
- 1 hour before breakfast, a glass of water at room temperature;
- at night 1 glass of fermented milk products (kefir, muesli, yogurt);
- prunes, dried apricots, figs;
-taking pre- and probiotics (lactomin and others);
-50 grams of lactulose dissolved in 500 ml of water to drink within 2 hours;
- taking a suspension of flaxseed;
- plantain seeds PlantagoOvate, Mucofalk 5.0 up to 3 sachets per day.
For colicky abdominal pain associated with IBS, take antispasmodics, regulators of intestinal motility: Duspatalin, Tribux, etc.
In the treatment of recurrent diverticulitis, drugs derived from 5-ASA (acetylsalicylic acid) should be periodically prescribed: salofalk, mesalazine, mesacol - 0.4-0.5. 1 tablet 3 times a day, 10 days every month for 6 months. These drugs can also be administered in the form of rectal suppositories, 250–500 mg 2-3 times a day. An antibiotic can be added to this treatment - 7 days a month for 3-4 months.
Treatment of acute diverticulitis and its complications
Uncomplicated acute diverticulitis is treated conservatively:
- maximum intestinal rest;
-antibacterial therapy (cefotaxime, ceftriaxone 2.0 2 times a day; metronidazole 500 mg 3 times a day;
- antispasmodics, analgesics;
— derivatives of 5-ASA.
If complications of diverticulitis occur, surgical treatment is indicated. This is in cases of perforation of a diverticulum with the development of peritonitis and the formation of an abscess, intestinal obstruction, severe intestinal obstruction, incessant bleeding, suspicion of colon cancer, ineffective drainage of an abscess in the presence of an intestinal-vesical fistula.
The scope of surgical intervention is individual for each patient.
PS All patients with diverticulosis of the large intestine should be warned that if persistent abdominal pain appears, body temperature rises to high levels, and general health deteriorates, they should urgently seek surgical help.
Zhukov Vasily Petrovich
Doctor of the highest qualification category
clinic No. 1
Chronic diverticulitis
Patients with chronic diverticulitis remain with persistent clinical symptoms despite standard treatment (pain in the left lower quadrant). It is considered atypical if systemic symptoms never develop. With systemic symptoms, chronic disease may manifest as a recurrent, intermittent acute illness or as a persistent illness with mild symptoms. It is often associated with cellulitis. If an infection occurs, inflammatory changes in the preparation will be visible.
Symptoms of diverticulitis
Patients with acute diverticulitis usually complain of pain in the left lower quadrant of the abdomen. However, patients with an elongated sigmoid colon and an inflamed segment may have pain in the right iliac region, masquerading as acute appendicitis. The pain is mostly constant, not colicky. Irradiation can be in the back, side on the same side, groin area and even in the leg. The pain may be preceded or accompanied by an episode of constipation or diarrhea. In general, the pain is progressive in nature if no treatment is applied.
Historically, age has been a priority factor in recognizing the most likely etiology of such pain. However, as the proportion of young patients with diverticular disease increases, the overlap of groups expands, which leads to the need to expand the diagnostic search in this group of patients.
Nausea and vomiting are quite rare in the absence of acute intestinal obstruction. Bleeding is a fairly rare symptom. The symptom of dysuria or false urge gives reason to suspect the involvement of the bladder in the inflammatory process or the formation of a colovesical fistula.
The presence of air in the urine, stool, or the release of gas and stool from the vagina gives reason to suspect the presence of a colovesical or colovaginal fistula, respectively. A fairly common symptom is fever, which is proportional to the body's inflammatory response. High fever is usually accompanied by perforation with an abscess or peritonitis.
Sometimes diverticular disease presents with rare symptoms, such as a chronic lower limb joint infection, when the fluid is cultured, intestinal bacteria are cultured from it. Other unusual manifestations include tumor-like changes in the projection of the left adnexa, inflammation, necrosis of the peritoneum and genitals, including Fournier's gangrene, subcutaneous emphysema of the lower extremities, neck and anterior abdominal wall, isolated liver abscess associated with intestinal infection, brain abscess caused by such same bacteria, skin disorders simulating pyoderma gangrenosum.
Complications of intestinal diverticulitis
In the absence of timely treatment for intestinal diverticulitis, many complications arise. First of all, the treatment will be difficult and lengthy. Conservative treatment methods are not effective and surgical intervention will be required. The rehabilitation period also increases.
Most patients self-medicate, taking painkillers until the situation worsens and the help of a medical specialist is needed.
Self-medication only worsens the condition and leads to negative consequences, such as:
The appearance of fistulas. In the absence of diagnosis and treatment, in addition to diverticula, fistulas form in the intestines. They penetrate the internal organs of the genitourinary system. This symptom is common in females. A purulent process opens. Internal organs become inflamed. Leads to infertility and other consequences.
Peritonitis. When a diverticulum becomes inflamed, it ruptures. The contents of the neoplasm pass into the abdominal cavity. The acute inflammatory process breaks down. If first aid is not provided, the situation can be fatal.
The appearance of adhesions. Scarring is observed in the intestines. The passages are blocked, which leads to intestinal obstruction. Feces stagnate in the body, the number of diverticula increases, and adhesions appear.
Peri-intestinal filtrate. The inflammatory process affects all internal organs. An infiltrate appears around the affected areas. Proctologists palpate it. The functionality of internal organs is impaired.
The appearance of cancer cells in the body. If left untreated for a long period, the inflammation of the diverticulum turns into a cancerous tumor. Cancer cells spread throughout the body and metastasize.
Diagnosis of colon diverticulosis
General X-ray of the abdominal cavity
The basic requirements for the results of a plain abdominal x-ray for suspected diverticular disease of the colon are to look for pneumoperitoneum or signs of intestinal obstruction, so the x-rays should be taken with the patient standing on the right or in the left lateral position. Computed tomography (CT) is the diagnostic method of choice for acute abdominal pain, so plain abdominal radiographs are rarely used in many medical centers.
CT scan
The great advantage of CT examination is the ability to document diverticulitis, even uncomplicated, when the clinical diagnosis is doubtful. It has been shown that CT can categorize patients into groups according to the severity of their disease. This study can differentiate uncomplicated disease with an expected short hospital stay from complicated diverticulitis, such as complicated abscesses, fistulas, peritonitis, or intestinal obstruction, with an expected long hospital stay. This study also provides information about lesions of extraintestinal organs and systems and anatomical variations that may be important for the choice of surgical tactics. Early CT-assisted drainage of abscesses can reduce the severity of complicated diverticulitis, transferring an emergency or urgent operation to a planned one. In some selected cases, surgery may not be necessary.
Colonography
Preliminary studies using MR colography have shown a high degree of agreement between the results and CT data in patients with diverticular disease in the absence of radiation to the patient. 3D modeling and virtual colonoscopy can only be performed outside the acute phase of diverticular disease of the colon. This careful 3D modeling, more than barium enema, can be instrumental in surgical planning with a critical assessment of the portion of the colon that should be retained during surgery.
Colonoscopy
Endoscopy in cases of acute diverticulitis should be used with extreme caution due to the high risk of perforation and the low likelihood of examining the cecum. In general, unless urgently indicated, colonoscopy should be delayed until symptoms of acute inflammation have resolved. When performing a diagnostic (routine) colonoscopy, the unexpected finding of an inflamed diverticulum (redness, swelling, pus or granulation tissue at the neck of the diverticulum) is quite rare and is observed in only 0.8% of cases.
To determine the location of diverticula, indications for surgery, as well as select the correct surgical treatment tactics, you must send me a complete description of the MRI of the abdominal cavity and small pelvis with contrast, if possible, colonoscopy data, indicate your age and main complaints by email. Then I will be able to give a more accurate answer to your situation.
Diagnostic methods
To more accurately determine the symptoms and prescribe treatment appropriate to the disease, a comprehensive diagnosis is carried out. It includes an external examination and instrumental studies.
When palpating the abdomen, diverticulosis is indicated by swelling and tenderness of the large intestine, especially in the left side, while there is no tension in the anterior abdominal wall.
Instrumental diagnostics for suspected diverticulosis include:
- intestinal irrigoscopy (x-ray using a contrast agent);
- colonoscopy;
- computed tomography or virtual colonoscopy;
- plain radiography of the abdominal organs.
Additionally, ultrasound diagnostics of the abdominal organs is prescribed. This study is carried out to exclude pathologies that are accompanied by symptoms similar to diverticulosis.
During diagnosis, it is important to exclude intestinal cancer or detect hidden diseases such as hemorrhoids, anal fissures, intestinal polyps and others. No less useful is information about the localization of formations in the large intestine and their current condition: the presence or absence of inflammation, bleeding, etc.
Treatment of acute diverticulitis
Initial treatment for asymptomatic diverticular disease consists of diet.
The goal of dietary manipulation is to increase fecal volume and thereby increase the intestinal lumen, reduce transit time and reduce intraluminal pressure. This reduces bowel segmentation, which has been described as a significant factor in the development of diverticular disease. The ideal amount of fiber is not known, however, the recommended amount is 20 to 30 grams. In general, fiber can be obtained by eating large amounts of food or by supplementing with one or more bulking (disintegrating) laxatives. Epidemiological evidence suggests that a diet rich in fiber may reduce the risk of developing diverticulosis.
Drug treatment for acute diverticulitis
In the absence of systemic signs and symptoms (high fever, marked leukocytosis, tachycardia, hypotension), most patients with symptoms of diverticulitis will respond well to fasting and outpatient antibiotic therapy. The diet is mainly slag-free or simply liquid throughout the entire acute phase and until the acute symptoms subside. Then an increase in the amount of fiber in food should be prescribed.
If general symptoms are noted, the patient should be hospitalized for more intensive care. Signs of more serious spread of disease include marked leukocytosis, high fever, tachycardia, or hypotension, as well as physical examination findings suggestive of intra-abdominal spread of disease requiring hospital treatment. Patients admitted to the hospital should usually be evaluated by CT scan, which can confirm the diagnosis, rule out other causes of similar symptoms, and evaluate for complicated disease that may require a change in course of treatment.
The main dominant microorganisms cultured from acute diverticular abscess and exudate during peritonitis are aerobic and facultative bacteria Escherichia coli and Streptococcus spp.
The most common anaerobes consist of
Bacteroides spp.
(B. fragilis group), Peptostreptococcus, Clostridium, and Fusobacterium spp. Antibiotics must be prescribed intravenously. Patients should not drink until signs of clinical improvement appear, which will make the likelihood of emergency surgery minimal. Symptoms should improve within 24-48 hours. Lack of improvement requires further diagnostic investigation, including repeat CT or surgery.
“Minimally invasive colon surgery”, K. V. Puchkov, D. A. Khubezov
Diagnosis of intestinal diverticulitis
It is extremely important to diagnose this disease in time. If discomfort in the intestines and other symptoms appear, you should contact a gastroenterologist and proctologist at the private proctology center “Proctologist 81 ”. The medical specialist obtains a medical history. You should inform your doctor about the nature of the pain, frequency, intensity, and symptoms.
With the help of palpation, a gastroenterologist can determine the exact size of the tumors . Next, the patient is sent for tests. These include a general blood test, stool, urine, and biochemistry. Sometimes you will need a blood test to check your glucose levels and to check for infections in your body.
After the tests are completed, instrumental examinations are carried out. We are talking about ultrasound examination and colonoscopy of the intestine. If there are no contraindications, computed tomography or magnetic resonance imaging is performed. To establish a diagnosis, a coprogram is taken from the patient and a stool sample is analyzed for the presence of bloody impurities.
Women must visit a gynecologist ; men should seek help from a urologist . X-ray examination of the intestine and laparoscopy are also performed.
Indications for surgical treatment for the acute phase of the disease
Indications for surgical intervention in acute illness include:
In an emergency requiring surgical intervention, simple disconnection with fecal diversion from the damaged segment of the colon, disconnection with suturing of the perforation site, obstructive resection (Hartmann operation) or with a mucous fistula (Mikulich operation) can be used. Additional measures include performing a thorough lavage of the abdominal cavity on the operating table.
In the acute setting, discussions of similar operations in the past have included a three-stage approach with disconnection, drainage, followed by a second-stage resection and a third-stage restoration of colonic continuity by anastomosis.
A modification of this approach involves suturing the visible area of perforation with tamponade of this area with an omental flap - as a primary operation. Alternatives consist of a two-stage approach consisting of a Hartmann or Mikulicz procedure followed by a second operation to restore intestinal continuity and resection with primary anastomosis, with or without a proximal protective stoma, in a single operation. For most cases, the entire debate revolves around the relative benefit of performing one-stage versus two-stage procedures in the acute phase requiring emergency surgery. The three-stage approach is least likely to be used unless the patient is extremely medically unstable.
Intra-abdominal abscesses
Patients who have an abscess need to have it drained percutaneously or transrectally, depending on its location. This is done to transfer the case from the plane of emergency surgery, with its inherent high mortality and the number of postoperative complications, to the plane of planned surgery.
If drainage cannot be performed without surgery, or if drainage is performed but cannot relieve the symptoms of abscess formation, then surgery is indicated. Although it is possible that intraoperative data from the revision will allow bowel resection with anastomosis, the most likely operation will be an obstructive Hartmann-type resection.
Therefore, based on these data, it is recommended that all patients with complicated diverticulitis undergo simultaneous elective surgery before complications develop.
Treatment of chronic diverticulitis and recurrent diverticulitis.
Most patients who report a first episode of diverticulitis symptoms have been symptom-free for at least 1 month before the onset of the disease. Most of them were helped simply by diet and outpatient antibiotic treatment. At least 10% of patients with a first episode of diverticulitis who respond to outpatient treatment will have a recurrence of the disease or continuation of symptoms that require hospital treatment. Then 20% or more of these patients will have a relapse of the disease. Some, but not all, will require readmission to the hospital.
The interval between acute episodes of inflammation can be extended to 5 years. After the second hospitalization, more than 70% of patients continue to suffer from these symptoms, and more than half of them require another hospitalization within the next year. The more severe the attack of inflammation, the more likely the disease will relapse.
Patients with multiple, repeated episodes of acute diverticulitis confirmed on CT should be candidates for surgery with colon resection.
Traditional training of doctors in tactics for diverticulitis dictates that patients who have more than 1 episode of uncomplicated diverticulitis undergo resection of the sigmoid colon. In fact, most data on resection performance were published before the introduction of CT scanning and modern antibiotics into clinical practice. Because of this and other studies, the American Association of Colorectal Surgeons has revised previous recommendations regarding resection for diverticulitis. The parameters of the 2006 revision are as follows: “the decision to recommend surgical treatment should depend on the age and general medical condition of the patient, the frequency and severity of attacks of diverticulitis, and whether persistent symptoms of diverticulitis persist after an acute attack or not.”
Surgical treatment of diverticular disease
The main goal is to perform elective rather than emergency surgery.
This requires correctly predicting which patients are most likely to have serious complications as a result of their disease. CT findings of complicated or “severe” diverticulitis provide some promise in predicting such risk. The risk of complications within 5 years after the first attack of diverticulitis exceeds 50% if CT data showed severe diverticulitis in the very first episode.
Elective surgical procedures include primary resections with anastomosis, resections with proximal colostomy, or obstructive resections (Hartmann procedure). Subtotal colectomy will also be performed.
Patients undergoing bowel resection for chronic disease are almost always candidates for the one-stage procedure with primary anastomosis. The American Association of Colorectal Surgeons' practice guidelines reflect several major recommendations regarding resection for diverticular disease. For elective resection, the entire thickened, diseased portion of the colon, but not necessarily all of the proximal colon where the diverticula are present, must be removed.
It may be acceptable to preserve the proximal colon with diverticula as long as the remaining colon is not hypertrophied. The entire sigmoid colon must be removed. When an anastomosis is performed, it must be applied to healthy rectal tissue, performed without tension and with good blood supply. The single most important factor in their recurrence after resection of the sigmoid colon for uncomplicated diverticulitis is the anastomosis to the sigmoid colon, and not to the rectum.
Laparoscopic surgery
Watch a video of operations performed by Professor K.V. Puchkov. You can visit the website “Video of operations of the best surgeons in the world.”
The role of laparoscopic surgery in the treatment of diverticular disease is increasing. Laparoscopic resections result in a short postoperative stay and fewer complications.
Despite the recent flow of literature and discussion of laparoscopic colectomies, only 5-10% of all colectomies are now performed using laparoscopic techniques. As evidence accumulates, it becomes clear that laparoscopic surgery is destined to play a large role in the treatment of diverticular disease of the colon.
All planned surgical interventions can be performed using laparoscopic access. And some of them using a single port (through one puncture).
Recurrence after resection
Recurrence of diverticulitis or its symptoms after resection is known in 3-13% of cases of elective surgery. Factors leading to relapse of diverticulitis are too short a resection area and anastomosis with the sigmoid colon rather than the rectum. The level of anastomosis is the only factor that reflects the risk of recurrence of diverticular disease after laparoscopic surgery.
- Ineffective treatment of phlegmon or abscess by non-surgical methods, confirmed by poor clinical indicators - an increase in fever, leukocytosis, tachycardia, hypotension, signs of sepsis or worsening of local manifestations (on physical examination).
- Perforation into the free abdominal cavity with peritonitis
- Intestinal obstruction
Useful links to various sections of the site on surgical treatment of colon diverticulosis:
preparation for surgery for colon diverticulosis... pain relief during surgery for colon diverticulosis... simultaneous (simultaneous) operations for colon diverticulosis... clinical databases... reviews of operated patients with colon diverticulosis... reviews of other medical specialists... scientific publications on colon diverticulosis …reports from journalists about the methodology of Prof. K.V. Puchkov
Complications of diverticular disease of the colon
- Diverticulitis.
This is an acute inflammation that occurs in the diverticula in a quarter of patients with diverticulosis. Signs of the development of inflammation may include the appearance of pain and muscle tension in the anterior abdominal wall, increased body temperature, chills, bloating, and bowel problems such as diarrhea or constipation.
- Diverticulum perforation.
Against the background of the inflammatory process in the diverticulum, part of its wall may collapse, and the contents of the intestine enter the abdominal cavity. In this case, local or diffuse peritonitis develops. When perforation (rupture of the wall) of the diverticulum into the retroperitoneal tissue or the space between the layers of the mesentery, infiltrates or abscesses appear.
- Bleeding.
Occurs in approximately 25% of patients with diverticular disease. For many people, it may be the first and only manifestation of the disease. Typically, bleeding is associated with ulceration of the diverticulum wall as a result of chronic inflammation. Also, at the site of the fecal stone, a bedsore may form with damage to the blood vessel. The intensity of bleeding can vary: from a slight admixture of blood in the stool (sometimes there is hidden bleeding, which is manifested by a gradual increase in anemia), to massive profuse bleeding, accompanied by collapse and even leading to death.
- Intestinal obstruction.
The cause of intestinal obstruction can be an inflammatory process around the diverticulum or an adhesive process, leading to deformation of the intestine and disruption of the movement of feces through it. In rare cases, intussusception (rolling in) of part of the intestine with a diverticulum or spasm of smooth muscles may occur.
- Intestinal fistulas.
They can occur when a diverticulum is perforated and an abscess breaks through into a nearby organ (the so-called “internal fistulas”). Men more often develop fistulas with the bladder, and women with the vagina. When an intestinal-vesical fistula forms, air or an admixture of feces may appear in the urine.