Indications for testing
It is difficult to imagine that a person who does not have symptoms of the disease would go for a full-scale examination unnecessarily.
Symptoms predisposing to testing for Helicobacter pylori:
- Gastralgia (pain in the stomach and intestines) of varying intensity. Appear during or after meals, caused by enzyme deficiency and impaired digestion of food and its stagnation in the stomach.
- "Hunger pains." They appear 2-3 hours after eating and disappear during meals. Due to damage to the mucous membrane, its sensitivity worsens, the patient feels how food and water pass through the digestive tract.
- Intense heartburn. It occurs due to the backflow of aggressive gastric juice into the esophagus that is not intended for this, and with frequent repetitions it is a symptom of pathology.
- A feeling of heaviness that occurs even after taking minimal portions of food. The patient has a feeling of a full stomach.
- Frequent nausea not caused by objective reasons (for example, toxicosis of pregnancy).
- A combination of stomach pain with vomiting and inability to eat and drink.
- Slight discomfort in the projection of the stomach, loss of appetite, mild heaviness. Often appear at the initial stage of heliobacteriosis.
- The presence of mucus in the stool.
Any of these symptoms is a reason to immediately consult a doctor for examination and treatment.
When is it worth testing for Helicobacter?
It is worth conducting a test for the presence of the bacterium Helicobacter Pylori in the body for any manifestations of problems with the digestive system. The following symptoms should alert you:
- frequent heartburn, belching of air or food;
- feeling of discomfort, heaviness, pressure in the stomach after eating;
- nausea after eating even in the absence of errors in the diet;
- aversion to meat food;
- sudden signs of metabolic disorders: brittle nails, increased hair loss, dry and flaky skin, unexpected allergic reactions.
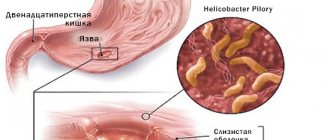
In addition, it is mandatory to conduct a test for Helicobacter if this infection has been identified in one of your family members, as well as in diseases such as gastritis, peptic ulcer, gastroduodenitis. Only after diagnosis, the doctor can prescribe treatment that will prevent the development of severe complications caused by Helicobacter infection. Please note that you cannot delay treatment, since the lack of therapy can lead to complications of diseases caused by this bacterium, namely gastric bleeding, perforation and penetration of ulcers, as well as malignant degeneration of erosions and ulcers.
Preparing for analysis
To obtain objective indicators, you need to carefully prepare for testing for Helicobacter pylori.
Necessary preparations:
- Complete smoking cessation the day before the test. Nicotine negatively affects the gastric mucosa, distorting test results.
- Complete abstinence from alcohol. The reason is the same.
- Prohibition on drinking tea and coffee, which negatively affect the gastrointestinal tract.
- Temporary restriction on food intake for 8 hours before analysis.
Since blood for Helicobacter testing is taken from a vein on an empty stomach, you can take some food and water with you to the clinic.
Breath test principle
The most popular method of diagnosing Helicobacter in modern medicine is the breath test. The urease helic test is based on the biochemistry of urea hydrolysis. Helicobacter produces urease during its life. This enzyme accelerates the conversion of urea into ammonia and CO2. Urease helps bacteria live and multiply in the aggressive environment of the stomach.
The patient is given a solution of carbamide (urea) to drink, the hydrolysis of which produces gas that enters the oral cavity. The level of gas entering the test tube before and after drinking urea allows you to determine the presence of bacteria.
The test shows the presence of helicobacter pylori and the level of contamination of the gastric mucosa. Repeated tests evaluate the dynamics of the disease.
Types of analyzes and diagnostics
There are several methods for studying the state of the body. Each of them has its own characteristics.
ELISA for bacteria
An enzyme immunoassay is prescribed to assess the level of concentration of antibodies to Helicobacter pylori in the patient's blood. If there are antibodies to the bacteria in the blood, it means that the immune system developed them at least 1-2 weeks ago. If the body's reaction has not yet been formed, a false negative result is possible.
Reasons for false positive results:
- error by the laboratory technician conducting the study;
- not enough time has passed after eradication, since antibodies are in the blood some time after complete cure.
A positive ELISA result indicates the need for a full examination, studying the results of an extended blood test, which provides more information about the condition of the body.
Immunoglobulins in the blood LgG, LgM, LgA
In the human body, when infections or pathogenic microorganisms penetrate it, immunoglobulins are produced - blood cell proteins that resist foreign viruses. When infected with Heliobacteriosis, the human body produces immunoglobulins LgG, LgM, LgA, which actively resist Helicobacter pylori. If they are detected in a person’s blood, it should be concluded that he is sick with heliobacteriosis.
The peculiarity of immunoglobulins is that in pursuit of pathogenic cells they overtake them anywhere in the human body. These proteins are produced after colonization by bacteria in the gastrointestinal tract.
Analysis transcript:
- A reduced or negative level of LgG immunoglobulin indicates one of the following options: the bacterium is absent in the body and the likelihood of developing a peptic ulcer is low, or only 3-4 weeks have passed since infection. If you have pain in the gastrointestinal tract, you need to repeat the examination in a week.
- An elevated or positive level of immunoglobulin LgG indicates one of two options: the bacterium is present in the body, increasing the risk of developing cancer and stomach ulcers, or the person has recently been cured of heliobacteriosis.
- A reduced level of immunoglobulin LgM, usually detected immediately after infection, or its absence, clearly indicates the absence of bacteria, since this protein is detected in the early period after infection.
- An increase in LgM levels indicates that the gastrointestinal tract is at an early stage of infection, and it is almost undamaged by the infection.
PCR analysis
The results of a polymerase chain reaction study can detect Helicobacter pylori DNA samples in the blood, which puts the PCR test in first place among all diagnostic methods. A positive test result proves the presence of bacteria in the body, a negative test shows its absence. The only thing that is not available when performing a PCR blood test is determining the time of introduction of the bacteria into the body.
If antibacterial therapy or antiseptic treatment was carried out before taking blood for analysis, the results of the study will not be objective. It is better to entrust the interpretation of blood tests to a specialist, although serious laboratories include a table of the norm and deviations from it in the results.
Cytological examination
In this test, swabs are taken from the antrum of the stomach during endoscopy. The area where the smear is taken is the area of edema and hyperemia, but not erosion or ulceration. After taking fingerprints, the laboratory technician dries and stains the smears.
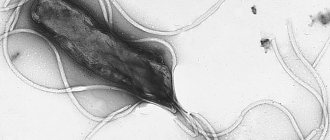
When examined under a microscope, Helicobacter pylori can be found in the form of a spiral or in the form of the wings of a flying seagull.
Cytology reference values:
- (+) — low level of contamination (up to 20 microbial bodies);
- (++) – average level (up to 40 microbial bodies);
- (+++) – high level (over 40 microbial bodies at 360x magnification).
Additionally, in the presence of inflammation, a cellular infiltrate is detected: (eosinophilia, neutrophilia, lymphocytes, plasma cells). Additionally, dysplasia, proliferation, metaplasia, and malignant neoplasms can be detected.
Urease test
The study is performed after taking a biopsy of the mucous membrane during endoscopy. It is placed in a carrier gel containing urea, a pH indicator, and a bacteriostatic agent. Conclusions are made based on the change in color of the biopsy material ranging from yellow to crimson.
Reference values:
- A crimson color appeared in the first hour – severe infection (+++);
- In the first 2 hours – moderate level of infection (++);
- By the end of the day – an insignificant level of infection (+);
- At a later date – the norm or a negative result.
With a low level of infection, a false negative result may be recorded. To increase reliability, it is combined with a histological method.
13C urease test, breath
This testing involves taking background breath samples on an empty stomach. After a light breakfast in the form of juice or milk, the subject drinks an aqueous solution of 13C-labeled urea, the so-called test solution. Then, 4 final samples are taken every 15 minutes.
Analysis of the test based on the presence of a stabilized isotope using a mass spectrometer:
- Mild infection - less than 3.5%;
- Average degree – 3.5-6.4%;
- Severe degree – 6.5-9.4%;
- Very severe degree - over 9.5%.
The norm for Helicobacter pylori in the urease test is 1%.
Hemotest
The analysis is based on determining the titer of antibodies - class G immunoglobulins. Normally, when Helicobacter enters the body, they bind microorganisms, stopping their pathogenic effect. The study is carried out by enzyme immunoassay after taking blood from a vein into a sterile tube. Before the study, you should not eat for 8 hours, drink coffee or alcohol, or smoke. To study the dynamics, the analysis is carried out throughout the entire treatment period.
Method 13C-UDT
It's time to figure out what a 13C-urease breath test is.
Breath tests for diagnosing Helicobacter pylori infection were first discussed in the late 80s of the last century, when Barry Marshall described the principles of this study.
Barry Marshall is a Nobel laureate. They proved that stomach ulcers are most often caused by the bacterium Helicobacter pylori.
According to these principles, conducting urease breath tests consists of administering a safe amount of urea to the patient and then analyzing the air he exhales for the presence of hydrolysis products of this urea. These products are carbon dioxide and ammonia. The presence of these gases in the exhaled air is a positive indicator of the presence of Helicobacter in the patient. In the case of diagnostics based on the study of carbon dioxide, the presence of isotopic markers in urea is assumed - carbon atoms 13C or 14C. The subject's breath is then analyzed for the presence of isotope-labeled carbon dioxide [1].
Let's turn to Wikipedia for more detailed explanations.
“The patient drinks a solution of the load - urea, labeled with the carbon isotope 13C. To improve the reliability of the test results, researchers recommend using a solution of citric acid or citrus juice.”
“For the study, two samples of exhaled air, taken before and after (30 minutes) taking the urea solution, are sufficient. Breath samples are collected in special bags, which are then transported to measuring equipment in analytical centers,” says the Internet encyclopedia [2].
Thus, 13C-UDT makes it possible to detect the presence of Helicobacter pylori. But when studying the materials attached to the instructions of domestic and foreign manufacturers of test kits, we come across a curious contradiction. Russian manufacturers delicately avoid some information that European manufacturers still provide. According to the latter, the 13C-urease breath test should not be used to diagnose patients with stomach ulcers, gastric infections and atrophic gastritis (which, by the way, can be caused by the desired bacterium), since these pathologies can affect the test result [3] .
Remember this when turning to domestic specialists: doctors may have no idea about these contraindications, and such diagnoses are not uncommon.
Nevertheless, some interesting points still await attentive people in section 11 of the instructions for the Russian test kit [4].
Impressive.
A number of questions immediately arise, which, unfortunately, remain rhetorical. Is it realistic to follow the required methodology in clinics and private clinics? How much do the physicochemical processes of the oral cavity affect the reliability of the result? Regarding the last point: what exactly is included in the concept of “physical activity”? Ten push-ups is obvious. Can jogging to the minibus and climbing the stairs to the fifth floor of the clinic also affect the result of the miracle test?
Decoding the analysis results
Despite the fact that the decoding of the indicators should be entrusted to the doctor who referred for the examination, all patients want to find out their results on their own.
How much is the norm for Helicobacter pylori? The norm of bacteria content when testing venous blood: 0-0.9 units/ml .
Interpretation of other meanings:
- 0.9-1.1 units/ml – the likelihood of Helicobacter pylori infection is doubtful;
- More than 1.1 units/ml – bacteria are definitely present in the body. High risk of developing stomach ulcers and stomach cancer.
The norm for the urease test is the absence of crimson color in the color of the material. The norm for bacterioscopic examination is the absence of pathogens.
In what cases is eradication therapy necessary?
I often hear from patients that they were prescribed eradication therapy based on the results of a positive rapid test for HP performed during FGDS. But the fact is that at present, when determining treatment and diagnostic tactics, gastroenterologists around the world are guided by a more complex test - Maastricht-4 (and several others). In this regard, the urease rapid test is preferably considered as an initial screening. If the doctor prescribed you eradication therapy only based on the results of FGDS, do not rush to take the drugs - it is better to do additional research to understand that this therapy is really indicated for you.
IgG antibodies to Helicobacter pylori
Detection of immunoglobulins to Helicobacter pylori is carried out using an enzyme-linked immunosorbent assay, or “sandwich” method. Venous blood is used for the study; you must not smoke for 30 minutes before donating it.
The method is based on the fact that after the Helicobacter bacteria enters the body, a local and systemic response develops. It consists of an increase in the titer of immunoglobulin IgM, IgG, and IgA antibodies in the blood serum. In 100% of cases of infection, IgG immunoglobulin is detected, in 65-80% of cases - IgA, in 17-20% - IgM, therefore, accurate diagnosis is carried out by determining the concentration of IgG in the blood serum.
Advantages of the method:
- Does not require endoscopy, so the method is safe;
- Highly sensitive;
- Used to prevent primary infection.
The method may not be accurate when determining the immunoglobulin titer in older people, since they have reduced antibody production, as well as in those patients who take cytostatics. After treatment of heliobacteriosis, this method is also not effective, because the level of the hormone in the blood after treatment with antibiotics remains quite high for another 6 months.
Indications for use:
- Patient complaints of dyspepsia when it is impossible to perform endoscopy;
- Primary diagnosis of heliobacteriosis;
- Monitoring the effectiveness of treatment with antibacterial drugs.
Reference values for the examination: IgG immunoglobulin concentration from 0 to 0.9, the result is negative. This may mean the absence of infection or high effectiveness of therapy.
The concept of "gold standard"
As mentioned above, you may hear from your doctor that the 13C breath test is a kind of “gold standard” in diagnosing Helicobacter pylori. Of course, for obvious reasons, domestic test kit manufacturers claim the same thing.
Indeed, European scientists studying Helicobacter pylori infection have organized a series of conferences with the participation of leading experts. Based on the standards of evidence-based medicine and a large number of controlled clinical trials, approaches to the diagnosis and treatment of Helicobacter pylori have been developed. The first conference was held in Maastricht (Netherlands) in 1996.
At the next conference, namely at Maastricht II, held in 2000, very optimistic recommendations were developed for the 13C breath test. The test has been presented as the best of the best for the primary diagnosis of helicobacteriosis, the so-called “gold standard”, with which others simply cannot stand comparison [5].
Almost 20 years have passed since then, and the concept of “gold standard” in relation to the 13C test has never been used again. Thus, at subsequent Maastricht conferences, the same scientists and doctors no longer put this method in first place among the others [6][7][8]. Firstly, this test is intended for primary diagnosis when endoscopy is not possible, and this happens extremely rarely. Secondly, even if it is the “gold standard”, it is exclusively for the control of eradication - the treatment of helicobacteriosis, but not for primary diagnosis [9]. However, in domestic sources the opinion of twenty years ago still prevails.
If Helicobacter pylori is positive, what does this mean?
A positive test result proves the presence of bacteria in the body, a negative test shows its absence. Positive indicators do not always indicate heliobacteriosis. Most often, this is a sign of the presence of bacteria in the body. However, immediately after eradication of Helicobacter pylori, the test for its content in the body will still be positive, despite the absence of the bacterium - antibodies in the blood do not disappear quickly. They are the ones who give a false positive result, so the test should be taken no earlier than a month after treatment.
This is the only exception to the rule: a positive result for Helicobacter means the presence of the disease or carriage of the bacterium.
How the research is carried out
The undeniable advantage of both types of breath tests is their non-invasiveness and comparative ease of implementation. They can be carried out both in a hospital setting and in a clinic.
Carrying out a C-urease breath test
Before starting the test, the patient is asked to drink 200 ml of orange juice (in case of an allergy to oranges, it can be replaced with apple juice). The patient is then seated on a couch or chair and asked to hold his breath for a few seconds. After this, you need to exhale into a special bag. Care must be taken to ensure that no saliva gets in there.
The bag is immediately sealed, after which the patient drinks a weak urea solution labeled with carbon isotopes C13 or C14. In order for the ingested reagent to spread throughout the gastric mucosa, the patient is often asked to lie on the couch and turn first on one side, and then lie on the other.
After about half an hour, the patient is again asked to exhale into a special bag.
When using urea labeled C14, air is taken once, and if urea with C14 is used, exhaled air is taken twice, with a ten-minute interval.
The finished samples are sealed, labeled and sent to the laboratory, where they are examined using a spectroscopic or spectrophotometric method. If the air exhaled after taking urea contains hydrocarbon vapors, this indicates infection with Helicobacter Pylori.
Carrying out a Helic test
To conduct a Helic test, the patient takes a sitting position, a tube with an indicator is placed in the examinee’s oral cavity, which is connected to a special digital device. The patient breathes into the tube for 7 minutes. The results are recorded by the doctor. You need to breathe normally, without “convulsive” inhalations and exhalations. It is important that the mouthpiece does not touch either the tongue or the palate, since the slightest amount of saliva entering the tube can distort the results. If saliva does get into the indicator, the study must be started again no earlier than half an hour later. Doctors recommend that if you really want to swallow, remove the mouthpiece from your mouth for a few seconds.
At the doctor’s signal, the patient takes 0.5 g of urea dissolved in 50 ml of water. This solution is colorless and tasteless, so no unpleasant sensations arise when taking it.
After this, the patient is again asked to breathe into the tube for six minutes and the results are recorded. Next, the patient takes the solution again and repeated tests are carried out.
Since no analysis materials are delivered to the laboratory, and the data is recorded by a specialist directly at the test site, Helic test results can be obtained very quickly.
Determination of Helicobacter pylori antigen in feces
The study is performed using the polymerase chain reaction (PCR) method. Its accuracy is 95%; determining the presence of bacteria in this way is recommended in children, elderly and seriously ill patients.
In order for the result of the analysis to be objective, you need to prepare for the study:
- Do not take antibiotics for 4 weeks before the test;
- 3 days before the test, do not eat foods that stain feces: red grape wine, beets, grapes, black currants;
- Before the study, 2-3 days before the study, exclude foods with coarse fiber from the menu: bran, radishes, cabbage, carrots, beets;
- Do not use medications that increase gastrointestinal motility.
For research, it is enough to fill a standard container for collecting samples one third full. You should not take feces from the toilet bowl, as it may contain traces of detergent. It is advisable to store the container with biomaterial for no longer than 10-12 hours at a temperature of +2 to -8°C.
The analysis result can be obtained the next day. Since stool analysis is a qualitative study, its result is formulated as “positive” or “negative”.
Test kit
Basically, the test kit includes a breath sample container and a load. The load is urea (urea) in powder form, and this powder is dissolved in water, with or without the addition of citric acid. More on this later.
Some researchers recommend using a citric acid solution or citrus juice to dissolve the load to increase the accuracy of the test results. But here, too, doubts arise: researchers have not agreed on whether it is worth dissolving the load in these liquids or whether it is better for the patient to drink these liquids before the procedure [10]. Since there is no single methodology, the point is extremely controversial. Apparently, people conducting this testing are forced to rely only on their intuition.
How do Russian test kit manufacturers answer this question? Today, three manufacturers of this type of product are registered in Russia. The HELICARB set, produced by .
recommends using orange or grapefruit juice in the study, but does not indicate in the instructions that, according to scientists, these drinks should be used with caution when testing patients with diabetes. In addition, many people are allergic to citrus fruits, and even a small amount of such juice can cause a corresponding reaction. Let us also remember that citrus juice has an aggressive effect on the gastric mucosa due to its high acidity. And since the test is taken by people with diseases of this organ, and on an empty stomach, taking an acidic liquid can become unpleasant (and even painful) for the patient. It is sad that the specialists conducting the test are forced to choose between the convenience of the patient and the reliability of the result. Another manufacturer, the creator of the “13C-CARBAMIDE-TEST” kit, even suggests using citric acid in the study, the effect of which on the stomach is also aggressive [11].
Let's figure out what else it offers us.
Dose of 13C-urea: 50 mg.
What does the instructions for the test kit itself say?
It turns out that an adult will take a child’s dose of the drug? The composition, of course, is expensive, and, apparently, this was the reason for the calculation of the dosage by the Russian manufacturer, which distinguished itself with its 50 mg. In the USA and Europe, the minimum dose of urea for this test has been approved, namely 75 mg [13].
Even more suspicious is the manufacturer's attempt to explain its own choice of dosage. Again, let's look at his instructions. Highlight:
“In order to optimize the dose of 13C-urea during 13C-UDT, we carried out a study in 2015... 23 volunteers took part... studied on a Heli View mass spectrometer (South Korea)” [11].
When conducting the study, the manufacturer assumed that the resulting optimal dosage of labeled urea would be used to test thousands, if not millions, of people. But how optimal was the number of subjects? Let me remind you: 23 people.
When conducting such studies, as a rule, the minimum number of patients is 200 people. This can be seen in a number of foreign publications of this kind [14][15][16]. Typically, authors of publications indicate diagnostic methods, with the results of which the results of 13C-UDT are compared. does not do this in his manual.
By the way, samples from these volunteers were examined on a “Heli View” device (South Korea), which is not in the state register of Roszdravnadzor, which deprives the manufacturer of this study of any credibility.
The manufacturer also refers to a Swedish company that produces test kits with the same (50 mg) dosage. However, these tests are produced in the form of tablets, and this eliminates the loss of load on the oral cavity and esophagus, that is, hydrolysis of urea occurs exclusively in the stomach. According to the Swedish manufacturer, this helps minimize false positive results [12]. However, among foreign manufacturers, such a dosage and form of loading is rather an exception. Accordingly, comparison is unacceptable.