Screening studies for colorectal cancer
Screening studies are diagnostic measures that are carried out in patients without symptoms of colon cancer. All these studies are divided into two types:
- Tests that can detect colorectal cancer and polyps. These methods assess the structure of the colon. For this purpose, endoscopic equipment or fluoroscopy is used. If a polyp is identified, it can be removed before it develops into cancer.
- Tests that are primarily designed to detect cancer. These methods are aimed at examining stool for signs of a malignant tumor in the intestine. These methods do not detect polyps.
Sigmoidoscopy
Sigmoidoscopy is an endoscopic examination that allows you to evaluate the inner surface of the rectum and sigmoid colon, the condition of their mucosa and identify the various presence of both polyps and malignant tumors, as well as perform a biopsy. In addition, this method allows you to identify other reasons for the presence of blood in the stool. A sigmoidoscope is used to perform sigmoidoscopy. It is a flexible probe with a light bulb and a camera lens at the end. The doctor can see the surface of the intestine with his own eyes. The length of the sigmoidoscope is approximately 60 cm, so the doctor can examine only the rectum and sigmoid colon.
Before performing a sigmoidoscopy, a cleansing enema is required. In addition, your doctor may prescribe a special diet for you to make it easier to prepare for the examination. Sigmoidoscopy takes on average 10-20 minutes. The procedure is painless and does not require anesthesia. The patient lies on a special table, on his left side, with his knees tucked to his chest. The sigmoidoscope is lubricated and then slowly inserted into the rectum. During the examination, the patient may feel some discomfort associated with the intestines distending with air.
Identification technique
When the disease relapses, the clinical picture is repetitive. It is assumed that the cause of the appearance of copious amounts of blood in the stool is radiation colitis or proctitis. Sharp pain in the lower abdomen accompanies ischemic colitis. High fever, gastrointestinal upset, chills, and abdominal pain are characteristic of ulcerative and infectious colitis.
If you have difficulty defecating or have thick stool, small anal fissures may appear. They promote the release of a small amount of blood. Malignant neoplasms can manifest themselves in frequent constipation or diarrhea, and stool irregularity. There are reasons to check your intestines.
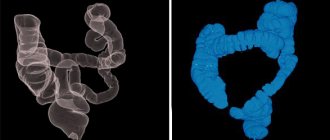
Patient's intestines
Examination of the anus may reveal anal fissures or hemorrhoids. They promote the release of a small amount of blood when going to the toilet. The patient is not limited to the examination. The doctor prescribes an additional examination, which may include examination by specialists.
The study can be carried out at any time during the course of the disease. At the very beginning of treatment, it will help confirm or refute the suspected diagnosis. Once confirmed, assess the extent of the disease and suggest methods and forms of exposure. Subsequently, it is used to assess the effectiveness of the chosen treatment method. At the last stage of treatment, it will help to choose the right forms of prevention and assess the quality of the course of treatment. Prevention of colon cancer is carried out for persons over 55 years of age once every three to five years. During this period, the polyp may mutate into a malignant neoplasm. A proctologist can develop an individual nutrition plan. Following a diet will significantly increase the reliability of the results obtained.
Indications for the procedure are:
- Colitis and cholecystitis;
- Irregular stools;
- Polyp formations;
- The appearance of blood in the stool;
- Preparatory stage for examination using the transrectal method;
- Intestinal dysbiosis;
- Enlarged prostate in men;
- Neoplasms or enlargement of internal female organs;
- Screening examination during preventive cancer examination.
There are a number of contraindications to the procedure. These are:
- The state of acute infarction and the six-month period after it;
- Impaired blood flow in the brain;
- Heart rhythm disturbances;
- The period after any surgical intervention.
Colonoscopy
Colonoscopy is similar in principle to sigmoidoscopy, the only difference being that it allows you to assess the condition of the mucous membrane of the entire large intestine, and not just its final sections. Colonoscopy is the same endoscopic examination. A colonoscope is used for this. This is a thin probe with a light bulb and a video camera at the end. The colonoscope also allows you to biopsy suspicious areas of the intestinal mucosa. Colonoscopy is performed, like sigmoidoscopy, with the patient positioned on the left side, with the legs tucked to the chest. Before inserting it into the patient's rectum, it is lubricated. Colonoscopy makes it possible to visually assess the condition of the entire large intestine, since the length of the colonoscope is 120–152 cm. During colonoscopy, as with sigmoidoscopy, a feeling of discomfort is possible. Colonoscopy also allows for a biopsy if a polyp or tumor is found.
Preparing for a colonoscopy
Careful bowel preparation is very important for colonoscopy. The study itself is usually carried out in the first half of the day. If necessary, the study can be performed in the evening. Before a colonoscopy, you need to switch to a slag-free diet 3-4 days before. On the eve of the study, the patient should not have dinner. In addition, two enemas are performed on the eve of the study at 20.00 and 22.00. On the day of the study, two enemas are also performed at 07.00 and 08.30.
Irrigoscopy with double contrast barium suspension
Irrigoscopy is a method of X-ray examination of the large intestine using a radiopaque substance - a suspension of barium sulfate, which is administered through the rectum. This is a completely painless procedure, it is non-traumatic and involves a lower radiation dose compared to computed tomography. Therefore, if there is a need for an X-ray examination of the large intestine, this technique is used. Irrigoscopy is indicated for bleeding from the rectum, intestinal discharge, pain in the anus, chronic constipation or diarrhea. It is also used to detect polyps and colon and rectal cancer. Preparation for irrigoscopy is the same as for other intestinal examinations.
The contrast agent for irrigoscopy - barium sulfate - is heated to 33 - 35 degrees. Carrying out irrigoscopy usually requires the use of not an enema, but a special device for intestinal lavage. The jar of the device is filled with contrast, and then the substance is pumped into the intestine with a bulb.
X-rays are taken as the intestinal lumen fills with a suspension of barium sulfate. After filling, a survey of the abdominal cavity is taken. The rectal tube is then removed and the patient goes to the toilet to have a bowel movement.
After the barium suspension has been released, another survey of the abdominal cavity is performed to visualize the intestinal mucosa and assess its evacuation function.
Irrigoscopy with double contrast is performed immediately after the end of the barium study.
Virtual colonoscopy
This is a type of CT scan that was developed to replace endoscopy. The essence of virtual colonoscopy is to conduct a CT scan of the large intestine. In this case, unlike colonoscopy or sigmoidoscopy, there is no need to insert a long probe into the patient.
The indication for virtual colonoscopy is to screen for polyps and other tumors in the colon at an early stage in order to remove them before they become malignant.
Preparing for a virtual colonoscopy
Virtual colonoscopy also requires bowel preparation. For this purpose, cleansing enemas are performed, or laxatives are prescribed. On the eve of the study, a slag-free diet is prescribed. Pregnant patients should notify the doctor performing the virtual colonoscopy before taking laxatives.
A virtual colonoscopy is performed like a regular abdominal tomography, except that air is introduced into the patient's rectum through a special tube to improve image quality and straighten the colon.
During the procedure, the patient is sometimes asked to hold his breath. First, the patient lies on his stomach, then he needs to roll over onto his back, sometimes vice versa. A virtual colonoscopy takes about 15 minutes. The entire procedure is painless, but there may be some slight discomfort from distending the rectum with air.
One week before the procedure
Ask questions about your medications
You may need to stop taking certain medications before the procedure. Talk to your healthcare provider about which medications you can stop taking. Below are some common examples.
Anticoagulants (blood thinners)
If you are taking a medicine to thin your blood, such as to treat blood clots or to prevent a heart attack, ask your doctor who prescribed it when you should stop taking it. The following are examples of common blood thinner medications.
Blood thinners
If you are taking blood thinners (which affect blood clotting), ask your healthcare provider what is best for you. Whether your doctor recommends stopping this medication depends on the type of procedure and the reason you are taking the anticoagulant.
| Examples of blood thinning medications: | |||
| apixaban (Eliquis®); | dalteparin (Fragmin®); | meloxicam (Mobic®); | ticagrelor (Brilinta®); |
| aspirin; | dipyridamole (Persantine®); | nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil®, Motrin®) or naproxen (Aleve®); | tinzaparin (Innohep®); |
| celecoxib (Celebrex®); | edoxaban (Savaysa®); | pentoxifylline (Trental®); | warfarin (Jantoven®, Coumadin®); |
| cilostazol (Pletal®); | enoxaparin (Lovenox®); | prasugrel (Effient®); | |
| clopidogrel (Plavix®); | Fondaparinux (Arixtra®); | rivaroxaban (Xarelto®); | |
| dabigatran (Pradaxa®); | heparin (subcutaneous administration); | sulfasalazine (Azulfidine®, Sulfazine®). | |
Medicines for diabetes
If you take insulin or other medications for diabetes, ask your healthcare provider who prescribed the medication what to do the morning of your procedure. You may need to change your dose before the procedure.
If you are taking metformin (such as Glucophage® or Glumetza®) or a medicine that contains metformin (such as Janumet®), do not take it one day before or on the day of your procedure.
If you are taking any other oral medications (medicines that you swallow) for diabetes, do not take them one day before or on the day of your procedure.
If you have an AICD, tell your healthcare provider.
Tell your Memorial Sloan Kettering (MSK) healthcare provider if you have an automatic implantable cardioverter-defibrillator (AICD). If you have this device installed, you must have the procedure performed at Memorial Hospital (MSK's main hospital).
If necessary, obtain a certificate from your doctor
- If you have an automated implantable cardioverter defibrillator (AICD), you will need to get a clearance letter from your cardiologist (heart doctor) before having the procedure. A certificate of admission is a document that states that this procedure is safe for you.
- If you have had chest pain, dizziness, trouble breathing, or fainting in the last 6 weeks, you will need to be seen by your doctor and cleared for the procedure before your procedure.
A certificate of admission to the procedure must be submitted to the MSK doctor's office no later than 1 day before the procedure.
Arrange for someone to take you home
You must have a responsible companion to take you home after the procedure. A responsible companion is someone who can help you get home safely and report problems to your healthcare provider if necessary. Agree on this in advance, before the day of the procedure.
If you are unable to find a responsible escort to take you home, call one of the agencies below. You will be provided with an escort who will take you home. There is usually a fee for these services and you will need to provide transportation. You can take a taxi or rent a car, but you need to have a responsible escort with you.
| Agencies in New York | Agencies in New Jersey |
| Partners in Care: 888-735-8913 | Caring People: 877-227-4649 |
| Caring People: 877-227-4649 |
Buy everything you need
- 1 (10 oz [300 ml]) bottle of magnesium citrate (magnesium citrate)
- 1 saline enema (such as Fleet® enema)
- Clear liquids
- Vaseline® or A&D® Ointment
to come back to the beginning
Fecal occult blood test
The essence of this research method is to identify “hidden” blood in the stool, which is not visible during microscopic examination. The presence of hidden blood in the stool indicates the presence of bleeding from any part of the gastrointestinal tract.
A fecal occult blood test is indicated if there is a suspicion of bleeding from any part of the gastrointestinal tract, which can occur, for example, with bleeding polyps or colon cancer.
Preparing for analysis
Typically, medications (especially bismuth and iron preparations) should be discontinued a week before a stool occult blood test. In addition, it is not recommended to perform enemas, and at least 2 days should pass after X-ray examinations of the stomach and intestines. Before performing a stool occult blood test, meat, liver, and all foods containing iron should be excluded from the diet.
After the procedure
The nurse will continue to monitor your heartbeat, breathing, and blood pressure. When you are fully awake, the nurse will remove your IV. Before you go home, your nurse will give you post-discharge recommendations.
At home
- Do not drink alcoholic beverages for 24 hours (1 day) after the procedure.
- Bowel movements may be accompanied by minor bleeding. This may continue for up to 24 hours after the procedure.
to come back to the beginning