What is gastroduodenitis? The insidiousness of gastrointestinal tract pathologies lies in the extreme diversity and nonspecificity of symptoms. Many signs are characteristic of several ailments at once. Thus, periodic nausea, an unpleasant taste in the mouth, belching or intestinal disorders may indicate both malfunctions of the duodenum and stomach problems.
An accurate diagnosis can only be made after a comprehensive examination. And after very unpleasant procedures, the doctor diagnoses gastroduodenitis. What it is and how to treat it is the patient’s first thought.
Causes
There are several causes of inflammatory disease, which are divided into two groups:
- endogenous;
- exogenous.
Endogenous causes are the basis for focusing on acid formation, disruptions in hormonal regulation of secretion, and a decrease in the level of mucus formation. A predisposition to gastroduodenitis is observed in patients with the following diagnoses:
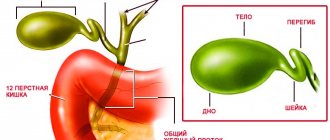
- diseases of the biliary tract and liver;
- endocrine pathology.
The most common exogenous etiological factors influencing the development of gastroduodenitis are:
- eating cold or hot, spicy food;
- chemical (exposure to pesticides);
- penetration of the bacterium Helicobacter pylori into the body.
How is gastroduodenitis different from gastritis?
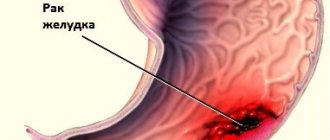
There are no significant differences between these pathologies: both gastritis and gastroduodenitis are inflammatory diseases of the gastrointestinal tract. The only difference is that gastroduodenitis has a wider area of damage to the mucous membrane than gastritis; it also affects the duodenum. A possible cause of the development of gastroduodenitis, gastritis and stomach ulcers is infection with the bacterium Helicobacter pylori. The diagnosis and treatment regimen for these diseases are practically the same.
Classification
Like any inflammatory disease, there are acute, chronic, and aggravated gastroduodenitis. Chronic gastroduodenitis is the most common; patients usually seek medical help in the acute stage. As a rule, a chronic process is a consequence of an untreated acute one, but the disease is often primary chronic, that is, it initially arises as a chronic disease, occurring with periods of exacerbations and remissions.
Depending on the nature of the pathological process occurring in the mucous membrane of the stomach and duodenum, the following forms of chronic gastroduodenitis are distinguished:
| Hypertrophic | the mucous membrane is hyperemic, in some areas there are hemorrhages (punctate hemorrhages), edematous, covered with a fibrinous-mucosal coating; |
| Surface | with this form, the mucous membrane of the stomach and duodenum is swollen, the folds are thickened; |
| Erosive | the mucous membrane is swollen, hyperemic, contains multiple erosions, covered with fibrinous-mucosal plaque. |
| Mixed form | the mucous membrane as a whole has the appearance of hypertrophic gastroduodenitis, but there are foci of atrophy; |
Depending on the secretory function:
- With reduced secretory function (reduced acidity);
- With normal secretory function;
- With increased secretory function (increased acidity).
The signs of the disease are extremely varied, and the form of their manifestation depends on the nature of the course; in acute gastroduodenitis they are bright, pronounced, but short-lived, in chronic gastroduodenitis they are constant, intensifying during exacerbations.
Possible consequences and prognosis for life
Acute erosions caused by food or toxic poisoning are best treated. They pass almost without a trace.
In a chronic process, especially one that lasts for a long time and is accompanied by bleeding, there is a high probability of ulcers forming. Long-term persistent treatment is required, sometimes many years. It is advisable to undergo endoscopy annually to understand the dynamics, as well as in connection with oncological alertness.
In continuation of the topic, be sure to read:
- Rectal fissure: causes, symptoms and treatment of pathology
- Causes of bloating and increased gas formation, treatment methods
- More about hemorrhoids: causes, symptoms and treatment methods
- Causes of abdominal pain: pathological and non-pathological cases
- Irritable bowel syndrome: symptoms and treatments
- Sigmoiditis (inflammation of the sigmoid colon): symptoms and treatment methods
- Rectal cancer: symptoms, stages, treatment and prognosis for life
- Details about the coprogram: preparation, conduct and interpretation of the analysis
- Typhlitis (inflammation of the cecum): symptoms and treatment methods
- More about Crohn's disease: symptoms and methods of treating pathology
Symptoms of gastroduodenitis in adults
Among the main clinical manifestations of gastroduodenitis the following can be noted:
- heartburn;
- burping;
- unpleasant taste in the mouth;
- pain in the stomach (the pain is often aching or cramping);
- nausea;
- decreased or loss of appetite;
- feeling of fullness in the stomach;
- constipation or diarrhea.
General symptoms may also be observed - irritability, increased fatigue, pale skin, dizziness, weight loss, sleep disturbances. During examination, the doctor may note tenderness of the abdomen upon palpation, a yellowish-white coating on the tongue with possible teeth marks. The tongue itself looks swollen.
If we talk about pain syndrome with gastroduodenitis, then it is characterized by increased pain after eating (usually this happens after 1-1.5 hours). In addition to nausea, heartburn and sour belching, vomiting may occur. Stool disorders are expressed both in the form of constipation and diarrhea.
Exacerbations of chronic gastroduodenitis usually occur in autumn and spring. This is largely due to the transmission of infectious diseases at this time, as well as nutritional disorders and increased psychological stress.
Symptoms of gastroduodenitis in children
Quite often, involvement of other organs (intestines, gallbladder, pancreas) in the process is observed, which greatly complicates differential diagnosis. The severity of symptoms of the disease in children is at a much lower level. All other aspects correspond to those in adults.
Pain in children usually occurs in the form of contractions. More often there is sleep disturbance, pallor, “bruises” under the eyes, loss of appetite, weight loss, mental instability, fatigue and retardation in physical development, brittle nails and hair loss (signs of hypovitaminosis), stool instability (constipation is replaced by diarrhea). Children with gastroduodenitis often experience autonomic disorders:
- vegetative crises that occur like dumping syndrome, causing drowsiness after eating;
- tachycardia (increased number of heartbeats);
- vascular instability;
- increased sweating;
- with a long gap between meals, signs of hypoglycemia may appear, dizziness, sweating, weakness, muscle tremors, and in exceptional cases, loss of consciousness may occur.
Exacerbations in adults and children are seasonal (autumn and spring). Their onset is provoked by neuropsychic or physical stress, and errors in nutrition.
Diagnostics
Based on the symptoms of the disease, additional instrumental and laboratory examinations are prescribed, which include:
- clinical blood test - indicates the presence of inflammation in the body (increased ESR and leukocytes);
- fibroesophagogastroduodenoscopy - a fiber optic tube with a camera and lighting is inserted into the stomach, the most informative method in which you can directly see the condition of the mucous membrane of the stomach and duodenum, the presence of erosions and their localization, if necessary, it is possible to take a biopsy (taking a tissue sample);
- Ultrasound examination (ultrasound) of the stomach - using a modern ultrasound machine, you can visualize the presence of an ulcer; it is used to exclude peptic ulcer disease;
- determining the level of acidity of gastric juice is a necessary study for choosing treatment tactics, since increased acidity in the stomach requires additional therapeutic measures;
- X-ray examination with a contrast agent (barium mixture) - the method allows you to see an ulcer filled with a contrast agent.
What is gastroduodenitis?
Gastroduodenitis
– inflammation of the mucous membrane of the stomach and duodenum. In fact, this is a more severe form of gastritis, in which the pathological process moves to the underlying organ - the duodenum, which can worsen digestive disorders.
Most often, gastroduodenitis is diagnosed in the age category of 30-35 years, and its symptoms are more similar to those of a peptic ulcer than gastritis.
Gastroduodenitis is divided into acute (short-term, recently developed severe pain) and chronic (systematic aching pain in the upper abdomen). In chronic gastroduodenitis, large-scale disturbances of secretory and motor-evacuation functions occur, followed by complete restructuring of the gastric mucosa.
Content:
Treatment of gastroduodenitis in adults
The basic principles of treating gastroduodenitis in the acute period include creating physical and psychological peace. Meals should be frequent (5 - 6 times), but in small volumes. Products that cause increased secretion of gastric juice are excluded from the diet: fatty, spicy, smoked, fried, and also containing extractives, spices and large amounts of fiber. The principle of the diet for chronic gastroduodenitis outside the acute period is the same, but it is more expanded and less strict.
Since one of the key causes of gastroduodenitis is infection, treatment cannot be done without antibiotic therapy. Drugs of choice for the treatment of gastroduodenitis in adults:
- De-nol and metronidazole (course of treatment 10-14 days) + tetracycline antibiotics (course of treatment 7-10 days);
- Clarithromycin and omeprazole in combination with metronidazole (course of treatment 7 days);
- Metronidazole + amoxicillin (course of treatment 10 days) + ranitidine (2 times a day before meals for 2 weeks);
- The choice of treatment regimen depends on the characteristics of the course of gastroduodenitis. At the first symptoms of gastroduodenitis, consult a gastroenterologist for advice and treatment.
Outside periods of exacerbation, physiotherapeutic treatment, balneological and spa treatment, and the use (after consultation with a doctor) of infusions of medicinal plants are recommended.
Causes of gastroduodenitis
There are endogenous and exogenous causes of the development of gastroduodenitis. With increased acid formation and low mucus production, and disruption of hormonal regulation of secretion, endogenous gastroduodenitis develops. Diseases of the liver and biliary tract, and disruptions in the endocrine system can also cause the development of gastroduodenitis.
Exogenous development factors include physical ones - for example, eating spicy, cold or hot foods, exposure to chemicals (pesticides). The penetration of the bacterium Helicobacter pylori into the digestive tract is also important.
The main causes of gastroduodenitis include:
- Poor or very fatty and spicy food;
- Non-compliance with food intake, dry food;
- Various stresses, psychological pressure;
- Helicobacter pylori infection;
- Infections that developed in the oral cavity and pharynx;
- Recently, it has been noticed that the causes of superficial gastroduodenitis may be a genetic predisposition to such diseases.
In addition, there are acute and chronic forms of gastroduodenitis, when periods of remission alternate with exacerbations.
Reasons for the development of acute gastroduodenitis:
- Toxic effects of chemicals and spoiled food, irritating the mucous membrane of the stomach and intestines;
- Consumption of hot spices and seasonings;
- High concentration of residual pesticides in food;
- Complications of intestinal infections and chronic somatic diseases;
- Increased production of hydrochloric acid in the stomach in combination with a decrease in the protective properties of the mucous membrane, occurring against the background of stress and poor diet.
Approximately 65-70% of cases of gastroduodenitis are a chronic form of the pathology.
Causes of chronic gastroduodenitis:
- Heredity;
- Helicobacter pylori infection;
- Complication of acute gastroduodenitis;
- Staying in constant stress mode;
- Poor nutrition with a deficiency of protein, vitamins and microelements;
- Dietary disorder;
- Diseases of other gastrointestinal organs (intestines, pancreas, gall bladder);
- Complications of somatic diseases (autoimmune and endocrine pathologies, blood diseases, liver and kidney failure);
- Side effects of drugs (NSAIDs, glucocorticosteroids) during long-term use;
- Smoking and alcoholism.
Each case of gastroduodenitis may have more than one reason for its occurrence. Several decades ago, after the discovery of the bacterium Helicobacter pylori in 1983, approaches to determining the etiology of this disease changed dramatically.
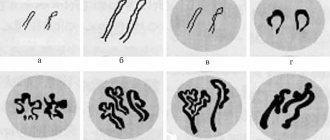
The flagella of active strains of pathogenic bacteria are able to penetrate through the epithelium of the gastric and intestinal mucosa damaged by it, and its enzymes break down the membrane proteins. Urease secreted by Helicobacter pylori disrupts microcirculation in the tissues of the gastrointestinal tract; hydrochloric acid ions damage the capillaries of the blood vessels of the stomach and intestines. All of these aspects contribute to the development of inflammation.
Normally, the bacterium is found in the gastrointestinal tract of almost every person, getting there in childhood.
Helicobacter pylori exhibits its destructive function due to a combination of the following factors:
- Violation of the nervous and endocrine regulation of gastrointestinal tract functions;
- Increased acidity of gastric juice and impaired production of its protection in the form of mucus;
- Imbalance of the ACUD system, which produces biologically active substances and hormones;
- Violation of the regenerative functions of the gastric and intestinal mucosa.
Treatment of chronic gastroduodenitis
Since chronic gastroduodenitis is characterized by a cyclical course of the disease, alternating exacerbations with periods of remission, treatment should be carried out in accordance with the following principles:
- during the acute period, the patient is prescribed bed rest, usually for at least 7-8 days;
- mandatory diet is required. Proper nutrition helps chronic gastroduodenitis respond more quickly to treatment and does not cause too much pain;
- if gastroduodenitis has led to increased stomach acidity, then patients are recommended to take omeprazole and H2 histamine receptor blockers;
- Physiotherapy, health resort treatment and exercise therapy show excellent results.
- To neutralize Heliobacter Pilori, drug therapy is carried out, which consists of taking bismuth tripotassium dicitrate, amoxicillin, macrolides and metronidazole. The treatment course lasts from 7 to 10 days.
In addition to the main medications, the doctor usually prescribes auxiliary agents for gastroduodenitis. The main purpose of these drugs is to reduce the side effects of drugs from the main group.
Among such drugs are antispasmodics, probiotics, vitamin complexes, as well as fixatives or laxatives. The entire course of treatment of gastroduodenitis with medications involves a significant load, which often negatively affects the functioning of other organs. Therefore, people often pay attention to traditional methods of treatment, which can be carried out together with traditional therapy.
Treatment
Since the duodenum plays an important role in the digestive system, its inflammation is particularly dangerous. Gastroduodenitis, as written above, affects not only the stomach, so it is worth preventing, but if the blow has already been taken, you need to start fighting it in every possible way.
Treatment of chronic gastroduodenitis is accompanied by the following measures:
- anti-inflammatory therapy;
- restoration of the secretory functions of organs involved in the digestive process;
- normalization of bile intake and secretion;
- eliminating imbalances in the nervous system, gastric lining and duodenum.
Thanks to modern treatment methods, it is possible not only to eliminate symptoms, but also to restore the health of the gastrointestinal tract, normalize digestion and absorption of food. Therapy is often carried out against the background of eliminating concomitant diseases.
- If there is low acidity, instead of antisecretory drugs that are aimed at producing hydrochloric acid. Regardless of the form, antacids are prescribed: Phosphalugel, Almagel, Maalox. For vomiting and flatulence, prokinetics are prescribed (Cerucal, Motilium). They restore the movement of the food bolus, eliminating painful symptoms.
- For diseases with high or normal acidity, proton pump inhibitors are used. These include Omeprazole, Rabeprazole, Neximum. There are other drugs that reduce the production of hydrochloric acid, reducing the acidity of gastric juice. Usually one medication is chosen for treatment.
If chronic gastroduodenitis is caused by a bacteria, then antibacterial drugs must be included in the treatment regimen.
Diet and nutrition rules
Without the use of this treatment method, drug therapy will definitely not bring the desired results. Table No. 5 according to Pevzner is used, which indicates what can be eaten with gastroduodenitis and what cannot be eaten. The menu of this table includes lean meats (beef, rabbit), poultry (chicken), vegetables, cereals, and dairy products. A prerequisite is that the preparation of these products is carried out by steaming, stewing is possible.
What is recommended to eat for gastroduodenitis:
- soups cooked in vegetable, mushroom, fish broths, pureed;
- soft-boiled eggs, omelet;
- lean meat (chopped, fried); boiled chicken;
- cutlets, steamed, stewed, fried, but without a rough crust;
- lean ham;
- boiled lean fish, chopped lean herring, pre-soaked, black caviar;
- porridge, boiled or pureed (buckwheat, semolina, rice);
- flour dishes: stale white, gray bread, dry crackers (exclude baked goods);
- vegetables, fruits, boiled, grated raw;
- vegetable and fruit juices;
- tea, coffee, cocoa with water and milk, marmalade, sugar;
- milk (if there is no diarrhea), butter, kefir, yogurt, cream, non-sour sour cream, fresh non-sour cottage cheese, mild grated cheese;
- Do not overuse tea and coffee: they promote the release of hydrochloric acid.
When eating, observe the following rules:
- Food and drink should not be too hot or too cold;
- You should never swallow solid food without chewing it thoroughly.
- It’s better to eat small amounts several times a day.
Proper nutrition consists of eating regularly in small quantities (at least 5 times a day). You can have dinner no later than 2 hours before bedtime.
Prognosis and prevention
Symptoms of gastroduodenitis are a serious reason to immediately begin treatment for the pathology, which can only be prescribed by a qualified doctor. Therapy for a chronic disease is a long process that requires patience.
Prevention consists of following the basics of a healthy diet, avoiding stressful situations, giving up bad habits and regular fasting/overeating. In addition, to prevent chronic pathology, it is important to minimize the use of medications, especially antibiotics.
Incorrect or untimely treatment of chronic pathology will cause a relapse of acute conditions. As gastroduodenitis develops, the patient’s quality of life will deteriorate and general fatigue will increase. Often chronic pathology is aggravated due to non-compliance with the regularity of treatment with prescribed drugs, which in the future can lead to complications, including peptic ulcer disease.
General Diet Recommendations
In general, the diet for gastroduodenitis looks like this:
- The first meal is oatmeal, semolina, buckwheat or rice porridge. You can have an omelette. For drinks, compote or juice is suitable.
- For the second meal, you can prepare a vegetable salad from potatoes, carrots, beets and cabbage. You can eat fruits and berries.
- Lunch should consist of a first and second course. For the first course, vegetable puree soups or cereal soups are suitable. The main dish can be boiled meat or fish with vegetable stew. Drinks – juice, compote, jelly, weak tea.
- An afternoon snack may include dairy (cottage cheese or kefir), baked apples, and a small amount of dried fruit.
- For dinner you can serve steamed fish and vegetables, cottage cheese casserole, cabbage rolls.
- Just before going to bed, you are allowed to eat some fruit or drink milk.
A proper diet for gastroduodenitis helps preserve all functions of the stomach and intestines and prevents the development of the disease. The dietary recommendations listed in the article are part of a healthy diet, so they can also be followed for prevention.
Folk remedies
Medicinal herbs cope well with the chronic type of disease and go well with the diet.
To get rid of the disease, decoctions are successfully used:
- yarrow,
- daisies,
- St. John's wort,
- dill seeds,
- valerian root,
- hops, etc.
In addition to homemade infusions, at the pharmacy you can buy special medicinal tea made from decoctions of motherwort, thyme, sage and medicinal chamomile. Herbal infusions help cope with the pain of gastroduodenitis during its exacerbation, and sometimes completely cure the disease, but, of course, subject to strict adherence to diet and medication.