Functional disorders of the gastrointestinal tract constitute a group of heterogeneous (different in nature and origin) clinical conditions, manifested by various symptoms from the gastrointestinal tract and not accompanied by structural, metabolic or systemic changes. In the absence of an organic basis for the disease, such disorders significantly reduce the patient’s quality of life.
To make a diagnosis, symptoms must exist for at least six months with active manifestations for 3 months. It should also be remembered that the symptoms of gastrointestinal tract can overlap and overlap each other in the presence of other diseases not related to the gastrointestinal tract.
Causes of indigestion
The reasons that influence the occurrence of FGD are divided into two types:
- The primary ones are irregular meals, snacking on dry food, eating large amounts of fried food and abuse of spices. Development can also be caused by bad habits – smoking and alcohol.
- Secondary (kidney and heart diseases, spinal pathologies, chronic infections, IOP-vegetative-vascular dystonia).
Primary causes most often cause stomach upsets in children, but can cause stomach pathologies in people of all ages. Secondary causes can also affect people of all ages.
Causes of functional disorders of the gastrointestinal tract
There are 2 main reasons:
- Genetic predisposition. FGITs are often hereditary. This is confirmed by the frequent “family” nature of violations. During examinations, genetically transmitted features of the nervous and hormonal regulation of intestinal motility, the properties of receptors in the walls of the gastrointestinal tract, etc. are found to be similar in all (or across generations) family members.
- Mental and infectious sensitization. These include acute intestinal infections, difficult conditions of a person’s social environment (stress, misunderstanding from loved ones, shyness, constant fears of various nature), physically difficult work, etc.
Symptoms
Symptoms of the disease in children and adults have minor differences.
Symptoms in adults
Attacks of aching pain, which are localized in the epigastric region, occur in most cases after eating.
Pain in the projection of the stomach is one of the clearest signs of pathology
May be accompanied by nausea, vomiting, and heartburn. The abdomen is painful and swollen on palpation. There is increased irritability, diarrhea, and decreased appetite. Rapid pulse, skin has a pale tint.
Symptoms of the disease in children
There is increased sweating, abdominal pain when pressed, and heaviness in the abdomen may develop. Belching with air (strong), frequent diarrhea. Slight increase in body temperature.
In children, functional indigestion is the most common, which is associated with poor nutrition (eating fast food), non-compliance with food intake and frequent psycho-emotional stress during the study process.
Symptoms of functional gastrointestinal disorders
Depends on the type of functional disorder:
- Irritable bowel syndrome (large and small) is a functional disorder characterized by the presence of abdominal pain or abdominal discomfort and combined with disturbances in defecation and transit of intestinal contents. To be diagnosed, symptoms must have existed for at least 12 weeks within the past 12 months.
- Functional bloating. It is a frequently recurring feeling of fullness in the abdomen. It is not accompanied by a visible enlargement of the abdomen and other functional gastrointestinal disorders. A bursting feeling should be observed at least 3 days a month for the last 3 months.
- Functional constipation is an intestinal disease of unknown etiology, manifested by constantly difficult, infrequent bowel movements or a feeling of incomplete release of feces. The dysfunction is based on a violation of intestinal transit, the act of defecation, or a combination of both at the same time.
- Functional diarrhea is a chronic syndrome with relapses, characterized by loose or unformed stools without pain and discomfort in the abdomen. It is often a symptom of IBS, but in the absence of other symptoms, it is considered as an independent disease.
- Nonspecific functional bowel disorders - flatulence, rumbling, bloating or distension, a feeling of incomplete bowel movement, transfusion in the abdomen, an imperative urge to defecate and excessive discharge of gases.
Diagnostics
There are several ways to accurately diagnose:
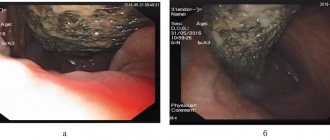
- gastric intubation - performed to determine the level of hydrochloric acid and the acidity of gastric juice;
- intragastric pH-metry - determines the characteristics of gastric juice secretion;
- esophagogastroscopy - helps to examine the motor function of the stomach, the presence of an inflammatory process, the presence of spasms or increased peristalsis;
- electrogastrography - used to study the bioelectrical activity of the stomach walls using an electrogastrograph;
- X-ray using a contrast agent (barium) - such a study makes it possible to assess the volume of the stomach, the tone of its walls, and the rate of processing of the contents;
- esophageal manometry - aimed at studying the contractile activity of the esophagus.
Diagnosis of the pathological condition is carried out only by a qualified specialist
Functional disorders of the motor and secretory functions of the stomach
Common signs of functional gastric disorders are:
- the connection between the occurrence of “gastroenterological” complaints and mental trauma, stressful situations or constantly existing traumatic factors;
- absence of signs of organic damage at the macrostructural and histochemical level;
- presence of neurosis;
- variability of symptoms, their disappearance at night, often distinguishing them from signs of diseases of the digestive system.
At the same time, the author notes that each sign and their combination are insufficient for diagnosing functional stomach disorders; they may be a manifestation of organic damage to the stomach or other organs.
The most characteristic symptom is pain in the epigastric region, in the right hypochondrium, near the navel (without clear localization). In addition, the location of pain may change over one or several days and may not be related to the intake or nature of food. The pain can be constant, aching or pressing, as well as acute, cramping like colic. Pain in the epigastric region may be accompanied by a feeling of heaviness, fullness, pressure, especially with secondary disorders of viscerovisceral reflexes in diseases of other organs (intestines, gall bladder, etc.).
The intensity of pain in the epigastric region depends on the personal characteristics of the patients, the severity of motor disorders of the gastroduodenal zone, and not on the secretory function of the stomach. More severe and prolonged pain, more often observed with increased gastric acid secretion, is associated with concomitant motility disorders in the form of spastic contractions of the pylorus, violent peristalsis, pendulum-like movements of the duodenum.
Antiperistaltic contractions of the stomach, especially with cardia insufficiency, lead to regurgitation of acidic gastric contents into the esophagus, irritation of the lower segment of the esophagus, the appearance of heartburn, and with strong contractions of the stomach - belching of sour, bitter air. When eating quickly, especially in neurasthenics, air is swallowed (aerophagia) and a very loud belch occurs. A “rotten” belch may appear when there is a violation of the evacuation of food from the stomach (pylorospasm, gastric atony, gastroptosis), when, due to rotting products of incomplete protein breakdown, hydrogen sulfide is formed and enters the oral cavity.
With motor and secretory disorders of the stomach, nausea may appear due to irritation of the vagus nerve, which is often accompanied by heaviness and pain in the epigastric region, salivation, unpleasant taste in the mouth, dizziness, and general weakness.
The occurrence of vomiting, often repeated, which does not bring relief, is observed due to reflex effects in diseases of other internal organs or irritation of the vomiting center. Indomitable vomiting of large quantities of acidic gastric contents, often accompanied by severe pain in the stomach, which is associated with habitual secretory neurosis.
Gastrosuccorea may also be characteristic of peptic ulcer disease with pyloroduodenal localization of the ulcer; it is characterized by continuous increased secretion of acidic gastric juice, profuse vomiting, heartburn, and night pain in the epigastric region. Both N. Reichmann's syndrome and gastrosucorrhea with pyloroduodenal ulcers can lead to hypochloremic uremia.
So, abdominal pain, heartburn, belching, nausea, vomiting are the most common symptoms of functional stomach disorders, but they are unique in these disorders, which, in combination with other symptoms, allows them to be differentiated from gastritis, duodenitis, and peptic ulcers. The clinical picture of functional disorders depends on their nature. Thus, with hyperchlorhydria and increased motor function of the stomach, sour belching, heartburn, vomiting, often with abundant sour contents, severe pain that does not have a specific localization, in combination with autonomic disorders, are more often observed. X-ray examination reveals increased gastric peristalsis, pyloric spasm, and delayed evacuation of gastric contents. Gastroscopy reveals abundant secretion, spastic contractions of the stomach, increased tone, which leads to frequent regurgitation of injected air. An increase in the tone of the smooth muscles of the stomach (frequent, high waves) is also noted by electrogastrography.
With hypo- and achlorhydria, anorexia, regurgitation of food, belching of air, bitterness in the mouth, nausea, sometimes vomiting mixed with bile and mucus, a feeling of heaviness and dull pressing pain in the epigastric region, often immediately after eating, dominate. Functional intestinal disorders are often associated; unstable stool appears with a predominance of diarrhea. The tongue is coated, swollen, with teeth marks along the edges, smoothed papillae, a hyperemic tip, in which a burning and tingling sensation is felt. Other signs of hypovitaminosis Bg (cheilosis), C (bleeding gums, gingivitis), A (dry skin, twilight vision disorder) are also detected. On palpation, in addition to gastroptosis, signs of intestinal irritation are often revealed - rumbling, splashing in the cecum and other parts (spasmodic areas). With a dynamic study of gastric secretion, heterochily is possible (increased acidity of gastric juice from low to normal and even excessively high) with preserved proteolytic activity of gastric secretion. X-ray examination reveals sluggish peristalsis, gastroptosis, pyloric dehiscence and rapid gastric emptying, i.e., signs of decreased tone. Sometimes, with a significant decrease in gastric tone, evacuation slows down. The decrease in tone is also visible on electrogastrograms: the waves are low, the intervals between them are significant. During gastroscopy, the mucous membrane is without pronounced changes, sometimes pale, there is a large amount of thick mucus in the stomach; possible admixture of bile.
In addition to disruption of the acid secretion and motor functions of the stomach, functional disorders include a decrease in mucus production, the most pronounced variant of which is amixorrhea, which occurs as a result of a decrease in the influence of the vagus nerve.
An attempt at a syndromic classification of functional disorders led to the identification of cardiospasm, pylorospasm, tetany, acute gastric dilatation, aerophagia, and habitual vomiting.
Cardiospasm often occurs with neuroses and thyrotoxicosis. Patients experience difficulty swallowing, chest pain, a feeling of food retention, and regurgitation. X-ray examination reveals spastic contraction of the cardial part of the stomach and the lower third of the esophagus.
Pylorospasm is also often observed in neurotic conditions, and is characterized by pain in the epigastric region, profuse vomiting of acidic gastric contents. With repeated vomiting, hypochloremic uremia may occur.
Tetany appears in patients with hypercalcemia associated with various causes. Its characteristic signs are convulsive contractions of the stomach muscles, repeated vomiting, acute pain under the xiphoid process, and gastrocardiac syndrome.
Acute dilatation of the stomach occurs in the postoperative period, with overeating, drinking large amounts of alcoholic beverages, including beer. The mechanism of occurrence of this syndrome is associated with paralysis of the neuromuscular system due to reflex or toxic influences, trophic changes in the stomach wall, and hypokalemia. Signs of acute gastric dilatation are sudden bloating of the abdomen, accompanied by a feeling of heaviness, fullness, pressure in the epigastric region, pallor, cold sweat, tachycardia and hypotension. It is rare at a young age; in acute myocardial infarction, thrombosis of gastric vessels, acute pancreatitis, peritonitis, it can cause death.
Aerophagia is observed mainly in people of the hysterical type, more often in women. When eating quickly or talking, these people swallow air, which leads to a feeling of bloating, fullness in the epigastric region and loud belching of air. These signs are the main clinical manifestations of this syndrome.
Habitual vomiting can occur with hysteria, neurasthenia, more often in young women; it sharply increases with neuropsychic stress and is associated mainly with neuro-reflex and conditioned reflex disorders of the motor function of the stomach by the sight, smell, taste of certain foods. Clinically manifested by vomiting or excessive regurgitation of food without preceding nausea, which occurs even after taking a small amount of food. These phenomena are caused by reverse gastric peristalsis, which easily occurs in response to certain foods in people prone to hysterical reactions.
Young men more often experience hypersthenic type disorders (“irritable stomach”), the causes of which in most of them are nutritional errors (77%), less often - previous diseases (20%) and only 3% - neuropsychiatric factors. At the same time, in young women, functional disorders of the hyposthenic type are more often observed, which are based on previous diseases (60%), including diseases of the central nervous system (20%). This is also associated with the more frequent occurrence of aerophagia, cardiospasm, and habitual vomiting.
Treatment
Basically, for the treatment of the pathology in question, it is not drug treatment that is primarily effective, but a change in lifestyle and eating habits.
Necessary measures for the formation of proper nutrition:
- normalize your diet - regularity of meals helps the timely production of the necessary enzymes and the required amount of gastric juice;
- careful selection of food products - high-quality products contain essential minerals and vitamins and are also easier to digest;
- mandatory consumption of liquid food (soups);
- do not overuse spices when preparing dishes;
- Minimize consumption of carbonated drinks and coffee.
Rules for a healthy lifestyle
To normalize the functioning of the stomach, it is very important to monitor your lifestyle:
- Correct work and rest schedule.
- Sports activities, you can simply walk more in the fresh air or add cycling in the park.
- Complete cessation of destructive addictions (smoking, drinking alcoholic beverages).
The doctor individually selects a treatment regimen for each clinical case
Treatment of functional gastrointestinal disorders
Complex treatment includes dietary recommendations, psychotherapeutic measures, drug therapy, and physiotherapeutic procedures.
General recommendations for constipation: abolition of constipation medications, foods that contribute to constipation, intake of large amounts of fluid, food rich in ballast substances (bran), physical activity and elimination of stress.
If diarrhea predominates, the intake of coarse fiber into the body is limited and drug therapy (imodium) is prescribed.
If pain predominates, antispasmodics and physiotherapeutic procedures are prescribed.