When can abdominal syndrome develop?
There is no general classification of this pathology. Its conditional division is based on the diseases in which it manifests itself. Abdominal syndrome (AS) is inherent in many diseases of the digestive organs: hepatitis, cirrhosis, pyloric stenosis of the duodenum and many others. Abdominal pain is also observed in diseases of the chest organs: pneumonia, myocardial infarction, diverticulosis of the esophagus. Even infectious and viral diseases can lead to the formation of abdominal syndrome (herpes zoster, syphilis). A special group of diseases in which the formation of abdominal syndrome (AS) is noted are diseases caused by metabolic disorders or pathology of the immune system, namely porphyria, diabetes mellitus and rheumatism.
The main clinical sign of abdominal syndrome is abdominal pain . The location of the pain can be anywhere; it is often not related to the anatomical position of the diseased organ. The pain leads to tension in the abdominal muscles. The pain may be accompanied by nausea, bloating, flatulence, diarrhea or constipation. Additionally, this symptom complex is joined by the symptoms of the underlying disease - fever during infection, heart pain during myocardial ischemia, arthralgia during rheumatism.
Children are a special risk group for the development of abdominal syndrome, which is associated with the ability of the child’s body to overreact to any damaging factor.
Treatment of pediatric functional abdominal pain
Includes a set of therapeutic measures aimed at eliminating pain. The child’s diet excludes foods that increase motor activity and gas formation in the intestines. Animal fats, chocolate, peas, beans, lentils, cabbage, milk, grapes, pickled vegetables, kvass, black bread, carbonated drinks, raisins are excluded. Fresh vegetables and fruits are limited.
To relieve pain, thermal procedures are used on the abdominal area (warm heating pad, warm fresh or sedative medicinal baths). If there is no effect, antispasmodic drugs are prescribed. Among myotropic antispasmodics, “Papaverine” is used, depending on age, 0.005-0.06 2 times a day; "Drotaverin" ("No-shpa", "Spazmol") for children under 6 years old, 0.01-0.02, from 6 to 12 years old, 0.02 1-2 times a day; “Mebeverine” (“Duspatalin”) at a dose of 2.5 mg/kg in 2 doses 20 minutes before meals (from 6 years); "Dicytel" 50-100 mg 3 times a day for school-age children. For flatulence, medications that reduce gas formation (Plantex, Espumisan) are prescribed. To normalize the intestinal microflora, pro- and prebiotics are used (Linex, Acitpol, Bifiform, Hilak-Forte). An important direction in treatment is the correction of the psycho-emotional state and consultation with a psychotherapist.
Essential drugs
There are contraindications. Specialist consultation is required.
- Papaverine hydrochloride (Papaverine) is a myotropic antispasmodic. Dosage regimen: 0.005-0.06 orally 2 times a day. For children aged 1 to 12 years, the maximum single dose is 200-300 mg/kg.
- Drotaverine (No-shpa) is a myotropic antispasmodic. Dosage regimen: for children under 6 years of age, when taken orally, the dose is 0.01-0.02, from 6 to 12 years, 0.02 1-2 times a day. The maximum daily dose when taken orally for children aged 6 to 12 years is 80 mg, for children over 12 years of age - 160 mg.
- Simethicone (Espumizan) is a drug that reduces flatulence, a carminative. Dosage regimen: for complaints related to excessive gas formation, adults and children over 6 years old are prescribed 2 caps. 3-5 times a day, possibly with a small amount of liquid, after each meal and, if necessary, before bed. The duration of treatment depends on the presence of symptoms of increased gas formation. If necessary, Espumisan can be used for a long period of time.
- Hilak forte (a drug that regulates the balance of intestinal microflora). Dosage regimen: for children, the drug is prescribed 20-40 drops 3 times a day; infants - 15-30 drops 3 times a day. After the condition improves, the initial daily dose of Hilak Forte can be reduced by half. The drug is taken orally before or during meals, diluted in a small amount of liquid, excluding milk.
| • | Leading specialists and institutions for the treatment of this disease in Russia: |
| Doctor of Medical Sciences, Professor, Head of the Department of Russian State Medical University, Professor Baranov A.A., Scientific Center of Health of the Russian Academy of Medical Sciences, Moscow. |
Types of abdominal pain.
Cramping abdominal pain (colic):
- caused by spasm of the smooth muscles of hollow organs and excretory ducts (esophagus, stomach, intestines, gall bladder, biliary tract, pancreatic duct, etc.);
- can occur due to pathologies of internal organs (hepatic, gastric, renal, pancreatic, intestinal colic, spasm of the appendix), functional diseases (irritable bowel syndrome), poisoning (lead colic, etc.);
- arise suddenly and often stop just as suddenly, i.e. have the character of a painful attack. With prolonged spastic pain, its intensity changes; after the use of heat and antispastic agents, its decrease is observed;
- accompanied by typical irradiation: depending on the place of its occurrence, spastic abdominal pain radiates to the back, shoulder blade, lumbar region, lower limbs;
- the patient’s behavior is characterized by excitement and anxiety, sometimes he rushes about in bed, takes a forced position;
- the patient often experiences accompanying phenomena - nausea, vomiting, flatulence, rumbling (especially when taking a horizontal position or changing position). These symptoms are important factors indicating dysfunction of the intestines, stomach, biliary tract or inflammatory processes in the pancreas. Chills and fever usually accompany dangerous intestinal infections or blockage of the bile ducts. Changes in the color of urine and feces are also a sign of blockage of the bile ducts. In this case, urine, as a rule, becomes dark in color, and feces become lighter. Intense cramping pain accompanied by black or bloody stools indicates the presence of gastrointestinal bleeding and requires immediate hospitalization.
Cramping pain in the stomach is an excruciating, squeezing sensation that goes away after a few minutes. From the moment of its onset, the pain takes on an increasing character and then gradually decreases. Spasmodic phenomena do not always occur in the stomach. Sometimes the source is located much lower. An example is irritable bowel syndrome. These digestive system disorders of unknown origin can cause pain, cramping, loose stools and constipation. People suffering from irritable bowel syndrome typically experience pain immediately after eating, which is accompanied by bloating, increased peristalsis, rumbling, diarrhea, or loss of stool. The pain subsides after defecation and passage of gases and, as a rule, does not bother you at night. The pain syndrome of irritable bowel syndrome is not accompanied by weight loss, fever, or anemia.
Inflammatory bowel disease (celiac disease, Crohn's disease, ulcerative colitis (UC)) can also cause abdominal cramps and pain, usually before or after a bowel movement and be accompanied by diarrhea.
A common cause of abdominal pain is the food we eat. Irritation of the esophagus (pressing pain) is caused by salty, too hot or cold food. Certain foods (fatty, cholesterol-rich foods) stimulate the formation or movement of gallstones, causing attacks of biliary colic. Consumption of poor quality products or food that has been improperly cooked usually results in food poisoning of bacterial origin. This disease is manifested by cramping abdominal pain, vomiting and sometimes loose stools. Insufficient dietary fiber or water can also be considered a leading cause of both constipation and diarrhea. These and other disorders are also often accompanied by cramping abdominal pain.
In addition, cramping abdominal pain appears with lactose intolerance - the inability to digest sugar contained in dairy products, with an autoimmune inflammatory disease of the small intestine - celiac disease, when the body does not tolerate gluten.
Diverticulosis is a disease that is associated with the formation of small pockets filled with intestinal contents and bacteria. They cause irritation of the walls of the small intestine and, as a result, not only spasmodic phenomena and cramping pain, but also intestinal bleeding can occur.
Another disorder that leads to pain can be a viral infection.
Pain from stretching of hollow organs and tension of their ligamentous apparatus
They are distinguished by an aching or pulling character and often do not have a clear localization.
Abdominal pain due to local circulation problems
Ischemic or congestive circulatory disorders in the vessels of the abdominal cavity.
- caused by spasm, atherosclerotic, congenital or other origin, stenosis of the branches of the abdominal aorta, thrombosis and embolism of intestinal vessels, stagnation in the portal and inferior vena cava system, microcirculation disorders, etc.
- angiospastic pain in the abdomen is paroxysmal;
- Stenotic abdominal pain is characterized by a slower manifestation, but both of them usually occur at the height of digestion (“abdominal toad”). In the case of thrombosis or embolism of a vessel, this type of abdominal pain becomes severe and increasing in nature.
Peritoneal pain
The most dangerous and unpleasant conditions are combined into the concept of “acute abdomen” (acute pancreatitis, peritonitis).
- occur with structural changes and damage to organs (ulceration, inflammation, necrosis, tumor growth), with perforation, penetration and the transition of inflammatory changes to the peritoneum.
- the pain is most often intense, diffuse, general health is poor, the temperature often rises, severe vomiting occurs, the muscles of the anterior abdominal wall are tense. Often the patient assumes a resting position, avoiding minor movements. In this situation, you cannot give any painkillers until examined by a doctor, but you must urgently call an ambulance and be hospitalized in a surgical hospital. Appendicitis in the early stages is usually not accompanied by very severe pain. On the contrary, the pain is dull, but quite constant, in the right lower abdomen (although it can begin in the upper left), usually with a slight rise in temperature, and there may be a single vomiting. The state of health may worsen over time, and eventually signs of an “acute abdomen” will appear.
- Peritoneal abdominal pain occurs suddenly or gradually and lasts for a more or less long time, subsiding gradually. This type of abdominal pain is more clearly localized; upon palpation, limited painful areas and points can be detected. When coughing, moving, or palpating, the pain intensifies.
Referred abdominal pain
We are talking about the reflection of pain in the abdomen during diseases of other organs and systems. Referred abdominal pain can occur with pneumonia, myocardial ischemia, pulmonary embolism, pneumothorax, pleurisy, diseases of the esophagus, porphyria, insect bites, poisoning).
Psychogenic pain.
This type of abdominal pain is not associated with diseases of the intestines or other internal organs - neurotic pain. A person may complain of pain when he is afraid of something or doesn’t want to, or after some kind of psycho-emotional stress or shock. At the same time, it is not at all necessary that he is faking it, the stomach can really hurt, sometimes even the pain is very strong, reminiscent of an “acute stomach”. But during the examination they find nothing. In this case, you need to consult a psychologist or neurologist.
Of particular importance in the occurrence of psychogenic pain is depression, which often occurs hidden and is not recognized by the patients themselves. The nature of psychogenic pain is determined by personality characteristics, the influence of emotional, cognitive, social factors, the psychological stability of the patient and his past “pain experience.” The main signs of these pains are their duration, monotony, diffuse nature and combination with pain of another localization (headache, back pain, pain throughout the body). Often, psychogenic pain persists after relief of other types of pain, significantly transforming their character.
Abdominal pain and intestinal pathology. Diagnostic issues, treatment approaches
Vladimir Trofimovich Ivashkin , academician of the Russian Academy of Medical Sciences, Doctor of Medical Sciences:
– Message from Marina Fedorovna Osipenko, professor from Novosibirsk.
Marina Fedorovna Osipenko , professor:
– Good afternoon, dear colleagues, dear Vladimir Trofimovich! The problem that I would like to discuss and touch on today concerns abdominal pain and intestinal pathology, issues related to diagnosis and treatment approaches. It seems to me that the fact that we began to discuss not only the nosological approach to patient management, but also the syndromic one, is actually very important, because especially for primary care doctors - and not only for primary care doctors, and for specialized specialists – patients do not come with a ready-made diagnosis, patients come with symptoms, syndromes, and, of course, our task is to verify the cause of these symptoms and syndromes, to build a nosological diagnosis. But on the other hand, our task is to ensure a certain quality of life for our patients even at the time of examination, and on the other hand, of course, to provide assistance in relieving symptoms and syndromes.
So, dear colleagues, you and I know very well that chronic pain - and in the vast majority of cases and most often we still encounter just such pain - affects 19-20% of the adult population. That is, almost every fifth person suffers from various manifestations or various causes, so to speak, underlying the occurrence of pain, and, of course, abdominal pain is one of the very serious symptoms for which our patients suffer greatly. Of course, we must remember very seemingly simple points, but they are very important so that you and I, in addition to identifying the abdominal pain itself, can also identify the causes of its occurrence. We all know very well from our student days that the mucous membrane does not have pain receptors, and accordingly, even severe lesions of the mucous membrane are often not accompanied by any pain. On the other hand, we understand that changes in pressure in the lumen of a hollow organ, which undoubtedly includes the entire intestine, lead to the activation of nociceptive receptors and the appearance of various pain sensations, just like the parietal peritoneum and mesentery , and in the end this is very, I emphasize once again, important, and you and I understand this, in order to verify the cause of pain.
Actually, it has long been clear that the level and threshold of pain perception is very different for everyone, and now a large amount of research in the world is devoted specifically to the genetics of pain, and more and more research concerns the enzymes involved in the metabolism of catecholamines and enkephalins, and features in the structure of the metabolism of opioid receptors, and genes that transfer afferent neurons, just like the genes that determine the transport of potassium, calcium, sodium ions, and so on. It is absolutely clear that in many respects the subjective perception of pain (and you and I perfectly understand that pain is a subjective manifestation of one or another degree of ill-health on the part of different systems and organs), it is determined precisely by a number of complex genetic factors, because one and the same In fact, a stimulus, if assessed even from some strict physical parameters, evokes completely different sensations in the patient. And we must, despite seemingly very banal things, clearly understand that in order to move from the syndrome to the actual nosological form, we must verify abdominal pain well enough and understand the possible mechanism of its occurrence.
We must find out the duration of the pain, we must find out its nature, we must find out its localization, we must try to determine whether its genesis is functional or organic, we must try to determine the mechanism of its formation, while taking into account and taking into account that in origin, despite localized in the abdominal area, this may not only be a pathology of the gastrointestinal tract itself, but it may also be manifestations from other systems and organs. Therefore, purely propaedeutic things were, are and remain very important in order for us to get out or move on, strictly speaking, to a diagnostic search. This is a necessary option for a normal diagnostic search. Of course, in most cases, we, gastroenterologists, and therapists in general, most often encounter subacute or chronic pain, that is, pain that lasts more than two days, let’s say. Acute pain in most cases is still the destiny of surgery, although any pain that later becomes chronic, it certainly begins at some point.
Of course, such moments as colic, which is still more associated with an increase in intraluminal pressure, or pain of an inflammatory nature, is more well localized, of a constant nature, more acute in the subjectivity of sensations, or ischemic in nature, with increasing intensity, aching , constant, around the clock - all this also helps us to verify the diagnosis in the same way as the localization of pain. If we are now focusing, or I am emphasizing in my message, on intestinal diseases that are manifested by abdominal pain, then we also know very well the places of localization of pain associated with the intestines - these are the lower abdomen or the right upper quadrant of the abdomen. The same important point is the attempt to determine the leading mechanism of the formation of abdominal pain, because we know very well that parietal pain is always the involvement of the peritoneal cover. It is clearly localized, it is accompanied by varying degrees of muscle tension, and the example that Vladimir Trofimovich gave at the very beginning of our round table once again emphasizes that the presence of parietal pain in the patient was not accompanied by the classic manifestations of this disease, but for all that in Ultimately, this situation turned out to be so. It intensifies with a change in body position, coughing, and, of course, if there is a suspicion that the pain is of a parietal nature, without a doubt, consultation with a surgeon and the surgeon’s participation in the management of patients must be mandatory.
Visceral pain - this is what we mostly encounter - this is precisely a change in pressure, stretching, tension, perhaps a circulatory disorder, this is the involvement of nosoceptive factors, and so on. In most cases, we are faced with precisely this genesis of pain. Referred, referred pain also gives us a lot of problems, since we often deal with it, and, of course, not arising in the place where the organ is projected, it gives us a lot of problems. Well, and, finally, psychogenic, which, essentially, we can diagnose only by the method of exclusion and with the help of completely different, very weak, let’s say, inherently tests. Of course, parietal pain is always an organic disease, without a doubt. As for organic diseases, in the initial stages, or rather, not even in the initial stages, but in the absence of complications, they can be accompanied by visceral pain. As soon as a reaction from the peritoneum occurs, it is, without a doubt, parietal pain.
Functional diseases are always visceral pain plus psychogenic pain, plus there may be components of radiating pain. The scope of examinations is different for all patients, and this, in fact, is a big task, because if all patients with abdominal pain are examined in depth using everything that is available in the world today, then, in general, not in any of the most developed civilized The country will not have enough such opportunities. Therefore, our task as doctors is, first of all, to outline for each patient, in each specific clinical situation, our own reasonable algorithm of actions and our own reasonable list of those examinations that will help us diagnose pathology. Of course, even such a method - I say “even”, because there was a time when a lot of people put their faith in laparoscopy and believed that this was a method that allowed practically, well, almost in 100 percent of cases, to reach the nosological form - in fact in fact, without a doubt, it has justified itself in this sense quite relatively, because a very specific list of nosological forms or pathological situations allows us to identify, and laparoscopy does not always allow us to get out, as I already said, and as you and I know very well , to a specific nosological form.
And now a review, in general, ten years ago, but quite correctly, let’s say, carried out, showed that from 10 to 15% of patients who underwent laparoscopy, essentially, were left, let’s say, without a definite diagnosis, because Laparoscopy was not helpful in diagnosing the cause of abdominal pain in these patients. Of course, today, gastroenterology especially is still a field of medicine in which the scope of the examination is largely determined by whether the patient has symptoms of anxiety or does not have these symptoms of anxiety. And you and I, understanding, on the one hand, the seemingly banality of these symptoms of anxiety and, it would seem, their obviousness, on the other hand, we must clearly understand that such moments as the nocturnal nature of pain, as the onset of the disease after 50 years , such as the presence of oncological or organic diseases in the family, if we are now talking about intestinal diseases, this is inflammatory bowel disease celiac disease, this is fever and loss of body weight, these are changes in direct examination of the patient, changes in the size of organs, these are changes in laboratory parameters - and routine ones, and the results of instrumental research methods, they force us, of course, to examine patients in more depth, because these are signals and markers of organic pathology. If we talk about intestinal diseases in general, then, of course, the most common cause of chronic abdominal pain is irritable bowel syndrome.
We all know the criteria very well, since they have practically not changed since 2006, and we understand that the leading one here is precisely recurrent abdominal pain, which is associated either with the fact of defecation, or with a change in frequency, or with a change in the shape of stool. And we perfectly understand that in order to diagnose irritable bowel syndrome, these are all the criteria that are listed and which are recommended to us by the Rome recommendations, all these criteria must be very strictly observed. Then, indeed, with a clear history and consistency of these symptoms, the likelihood of irritable bowel syndrome is high. This is visceral pain, and chronic, with a complete absence of anxiety symptoms. Moreover, it is chronic, that is, they arose, these pain sensations and these disorders, within six months. At the same time, we understand that despite the fact that this nosological form is called a syndrome, it is, in general, an independent nosological form, and issues related to the pathogenesis of its occurrence, the pathophysiology of its occurrence, are repeatedly discussed and very actively studied.
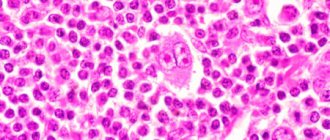
In doing so, we understand that if we clearly meet the criteria, the likelihood of irritable bowel syndrome—this is data relevant to previous irritable bowel syndrome recommendations—is 93%. However, irritable bowel syndrome can be masked, so to speak, or combined with some other diseases. These include enteropathies, inflammatory bowel diseases, parasitic colitis, lymphocytic/allergic colitis, bacterial overgrowth syndrome, diverticular disease, and endometriosis. Moreover, we must understand that there may be several options here. On the one hand, these may be similar syndromes of irritable bowel syndrome and intestinal diseases, and the second very important point is that there may be an overlap, that is, the presence of both intestinal diseases of an organic nature and at the same time irritable bowel syndrome. That is, when we encounter symptoms that are included in the criteria for the diagnosis of irritable bowel syndrome, we must understand that symptoms of another disease may be hidden behind them, or this may be the intersection of organic pathology and purely functional pathology.
If we consider approaches to the treatment of irritable bowel syndrome, there are a lot of guidelines. One that is fairly widely cited and not the most recent is the American College of Gastroenterology. Antispasmodics occupy a significant place there, they have a fairly good, let’s say, level of evidence, and it is m-anticholinergics that are predominantly discussed, and selective m-anticholinergics, when they talk about evidence-based therapy for IBS. But, however, if we are talking about what we must first differentiate irritable bowel syndrome from, then according to the recommendations of the World Gastroenterological Organization, celiac disease and parasitic diseases are most similar to IBS. Therefore, in patients with classic IBS manifestations, without symptoms of anxiety, we must exclude celiac disease, we must also exclude parasitic diseases. And then the most alarming from the point of view of other organic diseases are patients who have persistent diarrhea. Now, if we look at celiac enteropathy, today there are quite clear diagnostic recommendations in the world. They are based on determining, first of all, antibodies to transglutaminase, in addition, on determining the level of endomysial antibodies and the characteristics of the HLA system.
But in any case, when we talk about enteropathy, this is, of course, visceral pain, this is persistent diarrhea syndrome, this is the presence of varying degrees of melaabsorption, although melaabsorption may be absent, and extraintestinal symptoms that are characteristic of celiac enteropathy. Approaches to the treatment of celiac enteropathy in general are quite clear, although in some cases, in the presence of abdominal syndrome, we also always think whether this is an overlap with IBS or whether abdominal syndrome is somehow associated with the actual course of enteropathy, although in general this is not the most characteristic of this pathology symptom. If we talk about inflammatory bowel diseases, here, in fact, there may also be two classic situations, and mainly when we are faced with Crohn's disease due to obstruction or deep inflammation affecting the mucous membrane, submucosal layer, reaching the muscle layer, there may be a reaction with side of nociceptive receptors, so pain may occur, and the second option is, of course, crossover, the coexistence of these two nosological units. Here is the coexistence of two nosological units - studies have shown that in the population 30% of patients with ulcerative colitis suffer from IBS-like syndromes, with Crohn's disease this situation is more common.
And in one of Drossman’s latest reviews on inflammatory bowel diseases, IBS-like syndrome, in addition to the fact that we are trying to relieve pain by prescribing specific therapy for the treatment of inflammatory bowel diseases, we also use a different approach to treat pain, namely - inclusion of antidepressant drugs, antispasmodics and drugs that affect motor skills. The next nosological form that we include in the range of differential diagnosis is the syndrome of bacterial overgrowth in the small intestine. If we look and remember once again the symptoms that are associated with this pathology, we see many similar symptoms to irritable bowel syndrome. This is the same visceral pain, in most cases chronic, and symptoms of anxiety are not always present in these patients. In any case, a lot is now being said and written about the intersection of IBS with bacterial overgrowth syndrome, and it occurs in a large percentage of cases, and the important point is that, of course, there is specific treatment directly aimed at this bacterial overgrowth, but in a number of cases, we must also stop the manifestation of an IBS-like symptom complex in these patients.
The next situation, which is by no means rare, is diverticular disease, and at the same time, of course, in a number of patients it can be asymptomatic, in some cases we may encounter diverticulitis or other complications of diverticular disease, and finally, there is the term “symptomatic diverticular disease.” disease" is the presence of chronic abdominal pain, a violation of intestinal passage, which is very similar to the manifestation of irritable bowel syndrome. If we talk about the features of abdominal pain with diverticulitis, then we understand that this pain is visceral, with the addition of a parietal component, if we are talking about significant thinning of the walls of this diverticulum. As a rule, there are symptoms of anxiety - these are such as fever, such as accelerated ESR, such as increased levels of C-reactive protein. The pain, as a rule, is local, intensifies with movement, which indicates that the parietal component of this pain is attached, and, of course, age, without a doubt, is very important.
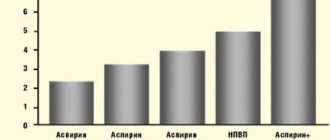
If we talk about symptomatic diverticular disease, the question is debated - whether it is segmental colitis, or whether it is simply concomitant irritable bowel syndrome. There are a lot of ideas expressed, but, indeed, it is very similar to irritable bowel syndrome in its manifestations, except, of course, for age. Since we understand that diverticular disease is the lot of people in older age groups, here, of course, age plays a very significant role in order for us to suspect this particular pathology in our patients. If we talk about approaches to treatment, then in uncomplicated acute diverticulitis, pain relief is an important section, and it is discussed in the guidelines that exist in individual countries. It should be understood that non-steroidal anti-inflammatory drugs worsen the course of acute diverticulitis, therefore the emphasis in treatment was placed on predominantly selective anticholinergic drugs - they reduce the pressure in the intestinal lumen - and drugs of the 5-aminosalicylic series.
As for the symptomatic form of management of diverticular disease, management is essentially no different from the management of patients with irritable bowel syndrome. And then there is a large list of various other inflammatory, allergic diseases of the intestines, both the small and large intestines. This group of diseases can never be discounted, and we have repeatedly encountered colitis, making a differential diagnosis of inflammatory bowel diseases, and there, for example, it turned out to be yersiniosis, and it, too, may not have a subacute, but a chronic relapsing course, and, of course, ischemic colitis , and, of course, associated with drugs, which we often forget about, and microscopic colitis. Despite the fact that, in general, I have not made many of these diagnoses in my life, it is certainly impossible to completely discount them. I demonstrate here some points, without focusing on particulars, that for each of the forms of colitis there are its own diagnostic features, and in many ways they are associated with features, including morphological histological conclusions. But as for, for example, some forms of microscopic colitis, here is a review from ten years ago, which suggests that distinguishing it from irritable bowel syndrome is not always really easy.
Well, and finally, new nosological forms appear, such as intestinal syndrome of drug addicts. Today, this form claims to be an independent nosological form, it occurs in people dependent on drugs, and this is associated with a change in the threshold of pain sensitivity, and, of course, we understand perfectly well that if it does not, then in the near future it will give us very There are many problems from the point of view of both managing these patients and making a diagnosis, among other things. Thus, in general, if we talk about approaches to the treatment of abdominal pain in intestinal diseases, of course, we should, in those cases in which we can, try to eliminate the cause. Although, alas, we cannot always do this. Next, of course, we must eliminate abdominal pain. It reduces the quality of life and makes it difficult to examine patients. There are a number of different approaches to this, and in general, if you arrange them in stages, then these are non-steroidal anti-inflammatory drugs, analgesics, antispasmodics, then more intense, let’s say, more complex opioid drugs and surgical interventions, these are, of course, antidepressants , and speaking here about antispasmodic therapy, we must understand: on the one hand, the combined prescription of drugs is indeed considered as one of the ways to relieve pain, but in this regard, hyoscine butyl bromide has its strengths, since it has a tropism for the enteric nervous system, and besides, here is a study that is good because for abdominal pain, the effect of paracetamol, the No. 1 drug in the world for pain relief, specifically for providing symptomatic assistance, showed almost completely similar results, and therefore we consider this drug as a drug for relief abdominal pain.
Moreover, taking into account that the frequency of side effects practically does not exceed the frequency of side effects when taking a placebo, and bearing in mind that pain of any origin is alleviated or stopped when using this drug, plus quickly, plus a small number of side effects, and that’s all , of course, we must take into account. Of course, we can use anticonvulsants, but it must be said that more research on this matter has been carried out specifically in chronic pancreatitis. In some cases, we can resort to laparoscopic treatment in situations where we suspect the presence of adhesions as the cause of pain, but we understand that these are not adhesions as such, but are either a reaction from the mesentery or changes in motility from the intestines. But if we look at the studies that are more or less rigorous today, then in no more than 60-70% of cases we have any lasting effect from this manipulation.
Thus, today we must clearly understand, and we know this with you, that abdominal pain is one of the most important symptoms of intestinal pathology, certainly not the only one, but very important. One of its causes, if we talk about statistics, the most common, is irritable bowel syndrome, and it can either be an independent nosological form, or it can hide an organic disease, or it can simultaneously coexist with an organic pathology. The mechanisms of pain are different, therefore they use different drugs, different combinations in pain relief, but it seems to me that we must clearly understand that pain relief in the 21st century is an independent clinical task, and we must do everything so that our patients, Living in this world, one should not experience this pain, including those suffering from serious illnesses. A large number of drugs are used, and various other approaches, including surgical, endoscopic, and one of the well-studied group of drugs that can relieve pain both in monotherapy and in complex therapy is a group of antispasmodics, and among them, of course, the important hyoscine butyl bromide takes its place due to its safety, fairly good study and thanks to those studies that have shown the safety of its use over long periods of time, up to 3 months. Thank you very much for your attention.
What should you do if you have abdominal pain?
If you have any abdominal pain, you should urgently consult a doctor - only he can determine the true cause of abdominal syndrome. Self-medication is fraught with serious complications. Abdominal syndrome may be one of the manifestations of an acute abdomen that accompanies peritonitis and requires surgical treatment. With the abdominal form of myocardial infarction, acute cardiovascular failure may develop. A general and biochemical blood test, ultrasound results, and radiography of the abdominal and thoracic cavity help the doctor determine the cause of AS. The patient himself assists the doctor in making a diagnosis, answering all questions in detail.
Diagnostics
Diagnosing the pathologies that caused abdominal pain is not always easy during an examination or based on patient complaints. To make an accurate diagnosis, laboratory and instrumental research methods are used.
Laboratory tests include:
- a general blood test, which evaluates the general condition of the body;
- a general urine test to detect pathologies in the functioning of the urinary system;
- biochemical blood test to determine the amount of enzymes, hormones and trace elements in the blood (including liver tests).
Instrumental diagnostic methods:
- Ultrasound of the abdominal organs;
- plain radiography with a contrast agent, with the help of which neoplasms and foreign bodies of the abdominal cavity are detected;
- computed tomography or magnetic resonance imaging. These studies are highly informative diagnostic methods. They are prescribed when the diagnosis cannot be established by other methods;
- ECG (if myocardial ischemia is suspected).
In what cases should you visit a proctologist for abdominal pain?
If the answer to at least one of the following questions is positive, you should consult a doctor:
— Do you often experience stomach pain?
— Does the pain you experience affect your daily activities and work responsibilities?
—Are you experiencing weight loss or loss of appetite?
— Do you observe changes in bowel habits?
— Do you wake up with intense abdominal pain?
— Have you suffered from diseases such as inflammatory bowel disease in the past?
— Do the medications you take have side effects on the gastrointestinal tract (aspirin, non-steroidal anti-inflammatory drugs)?
Diagnosis of abdominal pain (stomach pain).
1. All women of reproductive age must undergo a biochemical test to determine pregnancy.
2. Urinalysis helps diagnose genitourinary tract infection, pyelonephritis and urolithiasis, but is nonspecific (for example, in acute appendicitis, pyuria may be detected).
3. With inflammation, as a rule, there is leukocytosis (for example, with appendicitis, diverticulitis), however, a normal blood test does not exclude the presence of an inflammatory or infectious disease.
4. Results of liver function tests, amylase and lipase may indicate pathology of the liver, gallbladder or pancreas.
5. Visualization methods:
— if a biliary tract disease, abdominal aortic aneurysm, ectopic pregnancy or ascites is suspected, abdominal ultrasound is the method of choice;
— CT scan of the abdominal cavity quite often makes it possible to make the correct diagnosis (nephrolithiasis, abdominal aortic aneurysm, diverticulitis, appendicitis, mesenteric ischemia, intestinal obstruction);
— plain radiography of the abdominal cavity is used only to exclude perforation of a hollow organ and intestinal obstruction;
— ECG to exclude myocardial ischemia
— fibroesophagogastroduadenoscopy to exclude diseases of the esophagus, stomach, duodenum;
- sigmoidoscopy, video colonoscopy for suspected diseases of the large intestine
If a patient with abdominal pain examined according to the standards cannot be diagnosed (for abdominal pain of unknown origin), capsule endoscopy is recommended, since in this case abdominal pain may be caused by pathology of the small intestine (ulcers, tumors, celiac disease, Crohn's disease, diverticulosis, etc.). Difficulties in diagnosing lesions of the small intestine are due, first of all, to the difficult accessibility of this part of the digestive tract for standard instrumental diagnostic methods, the locality of the pathological changes that occur, and the lack of specific symptoms. Capsule endoscopy solves this problem and in most clinical cases helps to establish a diagnosis in patients with abdominal pain of unknown origin.
Classification of abdominal pain
Abdominal pain is:
- Spicy
. In this case, they are called colic. Very often, such painful sensations manifest themselves in attacks of varying intensity. Pain may appear suddenly and disappear just as quickly. Their occurrence may be accompanied by nausea, vomiting, flatulence, and palpitations. - Chronic
. Painful sensations are present almost constantly. Patients often characterize this symptom as “burning in the stomach.”
Acute pain
Acute abdominal pain in medicine is included in the concept of “acute abdomen”. This is a very dangerous symptom that indicates serious damage to internal organs. Diseases such as appendicitis, cholecystitis and pancreatitis during exacerbation, perforated ulcers, etc. cause acute abdominal pain.
In addition, this sign may indicate the possibility of developing other pathological changes:
- obstruction of hollow organs, in particular, the development of intestinal obstruction;
- impaired organ perfusion due to thrombosis, stenosis and ruptures;
- stretching of the capsule of a certain organ, for example, due to acute alcoholic hepatitis or heart failure.
Chronic pain
Chronic pain indicates the presence of serious pathologies in the abdominal organs. This pain syndrome most often occurs against the background of irritable bowel syndrome.
Chronic abdominal pain is of low intensity, but due to the fact that it is constantly present, a person is exhausted, irritability and depression occur.
In addition, there are other types of abdominal pain:
- Peritoneal pain. They are characterized by a sudden onset, last a long time and subside slowly. By palpation, you can accurately detect their location. Pain increases with coughing and sneezing.
- Abdominal pain of a cutting and pulling nature. They occur against the background of stretching of the muscles of the internal organs. In such cases, it is very difficult to find the location of pain using palpation.
- Stenotic and angiospastic pain. They occur against the background of impaired local circulation. In the first case, the intensity of the pain gradually increases, and in the second, the pain is paroxysmal in nature.
Differential diagnosis of abdominal pain (stomach pain).
Perforated ulcer of the stomach or duodenum - the patient suddenly feels extremely sharp pain in the epigastric region, which is compared to the pain of being hit by a dagger. Initially, the pain is localized in the upper abdomen and to the right of the midline, which is typical for perforation of a duodenal ulcer. Soon the pain spreads throughout the right half of the abdomen, affecting the right iliac region, and then throughout the entire abdomen. The characteristic position of the patient: lies on his side or on his back with the lower limbs brought to the stomach, bent at the knees, clasping his stomach with his hands, or takes a knee-elbow position. Severe tension in the muscles of the anterior abdominal wall, in a later period - the development of local peritonitis. Percussion determines the absence of hepatic dullness, which indicates the presence of free gas in the abdominal cavity.
Acute cholecystitis is characterized by repeated attacks of acute pain in the right hypochondrium, which are accompanied by elevated body temperature, repeated vomiting, and sometimes jaundice, which is not typical for a perforated gastric ulcer. When the picture of peritonitis develops, differential diagnosis is difficult; video endoscopic technology helps to recognize its cause during this period. However, with an objective examination of the abdomen, it is possible to palpate tense muscles only in the right iliac region, where an enlarged, tense and painful gallbladder is sometimes detected. Positive Ortner's symptom, phrenicus symptom, high leukocytosis, and rapid pulse are noted.
Acute pancreatitis - the onset of the disease is preceded by the consumption of fatty rich foods. Sudden onset of acute pain is of a girdling nature, accompanied by uncontrollable vomiting of gastric contents with bile. The patient screams in pain and cannot find a restful position in bed. The abdomen is swollen, muscle tension is like a perforated ulcer, peristalsis is weakened. Positive Voskresensky and Mayo-Robson symptoms are observed. Biochemical blood tests show a high level of amylase and sometimes bilirubin. Video endolaparoscopy reveals plaques of fat necrosis on the peritoneum and in the greater omentum, hemorrhagic effusion, and the pancreas with black hemorrhages.
Hepatic and renal colic - acute pain is cramping in nature, there are clinical manifestations of cholelithiasis or urolithiasis.
Acute appendicitis must be differentiated from a perforated ulcer. Since with a perforated ulcer, gastric contents descend into the right iliac region, it causes sharp pain in the right iliac region, epigastrium, tension in the anterior abdominal wall and symptoms of peritoneal irritation.
Thromboembolism of mesenteric vessels - characterized by a sudden attack of abdominal pain without a specific localization. The patient is restless, tosses about in bed, intoxication and collapse quickly develop, and loose stools mixed with blood appear. The abdomen is distended without tension of the anterior abdominal wall, peristalsis is absent. Pulse is frequent. A heart defect with atrial fibrillation is detected. Often there is an indication in the anamnesis of embolism of peripheral vessels of the aortic branches. During diagnostic video endolaparoscopy, hemorrhagic effusion and necrotic changes in intestinal loops are detected.
Dissecting aneurysm of the abdominal aorta - occurs in elderly people with severe atherosclerosis. The onset of dissection is manifested by sudden pain in the epigastrium. The abdomen is not distended, but the muscles of the anterior abdominal wall are tense. Palpation in the abdominal cavity reveals a painful tumor-like pulsating formation, over which a rough systolic murmur is heard. The pulse is increased, blood pressure is reduced. The pulsation of the iliac arteries is weakened or absent, the extremities are cold. When the bifurcation of the aorta and the mouth of the renal arteries are involved in the process, signs of acute ischemia are revealed, anuria occurs, and symptoms of heart failure quickly increase.
Lower lobe pneumonia and pleurisy can sometimes give a clinical picture of abdominal syndrome, but upon examination all signs of inflammatory lung disease are revealed.
Dangerous symptoms that require urgent surgical intervention for abdominal pain include:
· dizziness, weakness, apathy; · arterial hypotension, tachycardia; · visible bleeding; · fever; repeated vomiting; · increasing increase in abdominal volume; · absence of gas discharge, peristaltic noise; Increased abdominal pain; tension in the abdominal muscles; · positive Shchetkin-Blumberg symptom; · vaginal discharge; · fainting during defecation.
Principles of treatment of abdominal syndrome (AS)
In the treatment of abdominal syndrome (AS), priority is given to the treatment of the underlying pathology - normalizing metabolism, antibacterial therapy for infectious diseases. Painkillers are prescribed only after acute surgical pathology has been excluded. For vomiting, antiemetic drugs are prescribed, for constipation - a laxative, and for flatulence, digestive processes are normalized with diet and enzymatic preparations. Abdominal syndrome during myocardial infarction is relieved by the administration of narcotic analgesics, which eliminate pain but can cause vomiting.