What is OCD and how common is it?
Obsessive-compulsive disorder (OCD) is a mental illness that combines a group of obsessive-compulsive syndromes (symptom complexes) associated with obsessive thoughts and actions, which get their name from the Latin words obsessio (blockade, siege) and compulsio (coercion). To put it simply, obsessions are obsessive illogical thoughts, and compulsions are irrational actions imposed by them, which together are interpreted as an obsessive state. In fact, OCD is an obsessive disorder (OS), which is confirmed by the reduction in the ICD (International Classification of Diseases) of almost all types of obsessive disorders to the category of obsessive-compulsive disorder. Compulsions are obsessive, irresistible desires that are uncontrollable by a person, developing against his will and reason, causing negative emotions and often incompatible with his moral and ethical principles. Patients are aware of the wrongness and irrationality of their actions, but cannot resist them. The uncontrollability of compulsions by consciousness leads to feelings of fear, anxiety and the development of depression. In a broader context, compulsions are a wide variety of obsessive physical actions, often acquiring a ritual nature. Obsessive-compulsive disorder is characterized by multiple repetitions of psychopathological phenomena in the patient’s mind, accompanied by a feeling of involuntariness, compulsion, awareness of their irrationality and at the same time the failure of attempts to resist them. All these phenomena have a negative impact on the general emotional background, often causing depressive moods and reducing performance. At the same time, the patient has a critical attitude towards obsessive states. As for questions about the impact of OCD on intelligence, the answers in this case are ambiguous. Some authors believe that the obsessive state does not reduce the intellectual potential of the patient, others note cognitive impairment related to spatial and verbal memory, verbal fluency, and speed of information processing. NS is also differentiated depending on its location in the mental-emotional (phobia) and/or motor sphere (compulsion). These types of NS are practically never found on their own; in the human mind they are usually present in combination with each other, and in different proportions. If obsessive thoughts are difficult for others to notice, then compulsive actions are obvious and it is impossible to hide them from those close to you. In addition, NS can be divided into the following conditions: • Caused by specific and obvious psychogenic causes. • Having no apparent cause, so-called cryptogenic NS. OCD can occur as an independent mental disorder or in combination with sluggish schizophrenia, depression, epilepsy, after traumatic brain injury and in some somatic diseases. According to statistics, OCD affects 1 to 3% of the population, with the average age of hospitalized patients being 31.6 years, although the disease usually begins in adolescence and young adulthood (10-25 years). This indicates that a significant period of time passes between the onset of the disease and a visit to a specialist, on average about 7.5 years. At the same time, the majority of patients who consult a doctor for the first time are no longer able to study or work, and only a quarter of them can fully perform these functions.
Who is more likely to develop OCD?
Persons with a psychasthenic character are more prone than others to the occurrence of obsessive states - suspicious, superstitious, emotionally labile, prone to dramatizing events. In addition, factors such as: • Mental trauma and associated memories and experiences may be contributing factors to OCD. • Stimuli that coincide with those that in the past provoked feelings of fear. • Conflict situations that caused significant stress.
As for the hidden causes of OCD, they may be due to the mental characteristics of a particular person.
The neurochemical cause of the development of OCD is a change in the metabolism of neurotransmitters, in particular the synthesis and transmission of serotonin and dopamine. The identification of this etiological factor led to a revolution in the pharmacological treatment of OCD through the development of selective serotonin reuptake inhibitor (SSRI) drugs. There is evidence of a genetic predisposition to OCD - in 5-7% of patients, one or both parents also suffered from this disorder. Although the figure is small, it is still higher than that of the entire population. In addition, there are studies confirming the theory of the emergence and worsening of OCD symptoms due to streptococcal infection in the event of damage to nervous tissue.
Diagnosis of pancreatic lesions
In addition to confirming the symptoms from the patient’s words, palpating points and zones, it is necessary to take a biochemical blood test and assess the water and electrolyte balance. A urine test is required. To confirm the diagnosis, instrumental methods are needed to help examine the organ and identify pathological processes. An ultrasound examination is prescribed. To exclude the formation of stones, they are sent for an x-ray. Computed tomography and endoscopy help to provide an extensive analysis of the disease picture. It is important to start treatment in a timely manner.
What are the symptoms of OCD and what is characteristic of its clinical picture?
According to ICD-10, the basic signs of OCD are regularly recurring intrusive thoughts (obsessions) and compulsive actions in the form of peculiar rituals.
The clinical course is dominated by thoughts and memories associated with fear and anxiety. They are painful for the patient, alien to his thinking, and arise involuntarily, as if “from within.” The patient can fight them only by performing stereotypical ritual actions that relieve nervous tension and eliminate anxiety. After performing the ritual, the patient receives calm and relief for a while. But it does not last long - until the next occurrence of obsessive thoughts. By the way, to make a diagnosis of OCD, the duration and frequency of occurrence of obsessive states are important. If it takes more than 1 hour a day to perform ritual actions in total for 1-2 weeks or more, then we can talk about the presence of obsessive-compulsive disorder.
As I already said, the initial stage of development of OCD usually occurs in adolescence and young adulthood (10-25 years). Moreover, it is during this period that the most pronounced clinical picture of the disease is observed, the main manifestations of which are the following symptoms: 1. The presence of obsessions - fleetingly arising painful thoughts, ideas and images that forcibly invade a person’s thinking, which he is trying to resist. This confrontation between the occurrence of obsessions and attempts to fight them can cause deep internal conflict in the human psyche. The form of obsessions can be very diverse - individual words, phrases, poems, song verses, images, scenes, etc. Moreover, they can be quite shocking, lustful, obscene and disgusting. 2. The emergence of obsessive stimuli - urges to commit certain actions, including dangerous, shameful and even sadistic. For example, running across the road in front of moving traffic, undressing in a public place, shouting obscenities, or even hitting a child.
3. Performing obsessive rituals, of which there can be two options: • Mental in the form of mental repetition of a count or certain words. In this case, counting is often combined with words. For example, say the words “nothing will happen” or “everything will be fine” 6 times, and repeat this procedure three times. And also end with a verse of some unknown reason chosen song or poetic lines. The ritual is quite complex and demanding, because at the slightest failure it must be repeated, otherwise, in the opinion of the patient, it will lose its effectiveness. • Physical actions that are sometimes striking in their absurdity. For example, if washing your hands too often can be explained by the fear of infection, then looking in the mirror a certain number of times before leaving the house has no logical basis. Over time, rituals can become more complex and become a problem in everyday life and at work. 4. Internal obsessive discussions regarding the arguments for and against certain actions. Obsessive doubts can concern even the most simple situations, for example, turning off household appliances, locking locks, fear of hitting someone while driving, remorse due to non-compliance with religious requirements, or the use of obscene language. 5. Perfectionism - the desire for order and symmetry, when everything should be perfectly ordered and located in its place. 6. Compulsions – regular repetition of actions that are protective and preventive in nature in relation to even the most unlikely situations that are potentially dangerous for the patient himself and his family. Often patients in this case avoid the circumstances and places with which their fears are associated. For example, kitchens where knives are located or workshops with piercing and cutting tools. It is difficult to imagine the torment of a housewife who is afraid to be in her own kitchen or a professional seamstress who is afraid of scissors and needles. 7. Superstition, exaggerated attention to everything that may be associated with good or bad luck.
8. Obsessive fears (phobias) up to panic attacks. All these psychopathological phenomena are accompanied by varying degrees of anxiety, which all obsessive and compulsive rituals are aimed at reducing. To assess the severity and dynamics of the clinical picture of OCD, the so-called Yale-Brown scale is used. It consists of 10 points that the patient must answer during a conversation with the doctor. Answers are scored on a five-point scale from 0 to 4 and cover a one-week period. The sum of the obtained indicators allows us to differentiate the severity of OCD symptoms, for example, a sum of up to 7 points indicates a subclinical course, and 32-40 points indicate an extremely severe course of OCD. Comparison of weekly indicators allows us to evaluate the effectiveness of treatment and the course of the disease over time. It should be noted that adapted versions of the Yale-Brown scale have been developed for the patient’s self-assessment of his mental state.
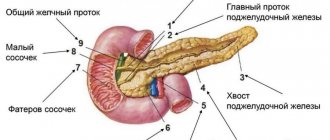
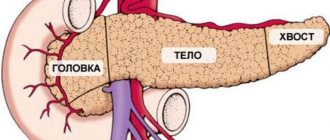
The structure of the pancreas
This large organ is located on the back wall of the abdomen behind the stomach. It consists of three branches:
- The head is hook-shaped.
- The body is similar to a prism, separated from the head by grooves.
- The tail of the pancreas, the end of the body, is slightly curved upward.
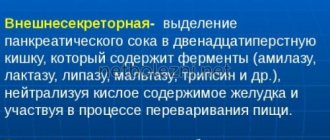
The pancreas occupies an important place in ensuring the vital functions of the body, and is also responsible for performing external and internal secretory activities. When it is damaged and there is an inflammatory process, a disease such as pancreatitis occurs. In appearance it can be acute or chronic. Inflammation of the pancreas can cause other diseases.
Patients often experience pain on the left side under the ribs. Other signs of pancreatic disease may appear after some time. This is sudden weight loss, loss of appetite, vomiting, diarrhea. The patient may not be aware of the inflammatory process. Therefore, if you experience periodic pain on the left side under the ribs, you should contact a medical facility to find out its cause. Damage to the pancreas can lead to serious consequences.
What types of obsessions exist and how do they manifest themselves?
Differentiation of obsessions (obsessions) is of practical importance for diagnosis and choice of treatment. Read more about Gestalt therapy. In modern psychiatry, the following types of obsessions are distinguished: • Obsessive doubts - constant uncertainty about committing or not committing certain actions. For example, whether the door is locked or not, whether the iron or gas is turned off, the form may have been filled out incorrectly or the details on business documents have been mixed up, the instructions from the authorities have been carried out correctly or not, etc. It is characteristic that repeated checks do not lead to getting rid of doubts, but only give rise to increasing uncertainty in oneself and one’s actions. • Intrusive memories of sad, unpleasant or shameful events associated with feelings of shame and remorse. They literally dominate the patient and interfere with an adequate response to current events. • Obsessive urges that encourage you to commit dangerous, cruel, and sometimes sadistic acts. This is the most destructive type of obsessions that cause the patient fear and horror from the failure of attempts to get rid of them. An example could be the desire to throw yourself or push a loved one under the wheels of a moving vehicle, physically abuse your wife, or kill your own child. The fear of carrying out such actions can be classified as one of the most painful phobias. • Obsessive ideas constitute a fairly diverse group of obsessions and concern either a figurative vision of the results of one’s own or someone else’s cruel behavior, or the perception of implausible, sometimes absurd situations as if they actually happened. For example, a patient may be convinced that his loved one was buried alive, imagines all the suffering of a person buried alive and is tormented by this. As the disease progresses, a person ceases to distinguish between reality and fiction, and is finally convinced of the correctness of his ideas, which translates obsession into the category of extremely valuable delusional ideas. • Obsessive antipathy towards certain people - relatives, respected persons, clergy and even saints. This irrational antipathy is associated with cynical, blasphemous thoughts towards them, sometimes even inciting violent actions. • Obsessive phobias, expressed in an inexplicable fear of heights, crowds, open or enclosed spaces, sudden death, incurable disease, etc. Very rarely, phobias multiply like mushrooms after rain and acquire the character of panphobia, when a person is afraid of everything. In addition, such a paradoxical effect as the emergence of an obsessive fear of developing fears (phobophobia) is possible. Obsessions are also differentiated into such types as: • Obsessions of neutral content, which include obsessive counting, memories of terms, insignificant situations, obsessive thoughts on neutral topics, etc. • Contrasting, otherwise aggressive obsessions, which manifest themselves in the fear of harming oneself or loved ones, in blasphemous thoughts and/or sadistic ideas. Such obsessions are completely alien to the patient’s consciousness, are not motivated and are accompanied by strong affective manifestations. • Obsessions with contamination and/or contamination (mysophobia). This group includes a variety of obsessive fears of contamination by dust, soil, excrement, toxic substances, and pathogens. The latter has become especially relevant today in the era of the coronavirus pandemic. In addition, people are afraid of small objects, such as glass shards or needles, entering the body. Preventive measures on the part of the patient often do not usually attract others, especially when frequent washing and wearing masks become justified and necessary in an epidemic. But when they acquire hypertrophied and irrational forms, it is no longer possible to explain them by excessive cleanliness or disgust. When a patient, under normal living conditions, without a real threat of infection, continues to observe the maximum security regime, does not leave the room and does not even allow loved ones near him, this already threatens complete desocialization and is not justified by the force of habit. Here you need the help of a specialist. The list of the most common obsessions includes isolated monophobias in the form of movement disorders, most often originating from childhood. These can be such familiar phenomena as: • smoothing imaginary falling hair, which actually lies perfectly in the hairstyle; • getting rid of an imaginary speck in the eye by blinking; • habitual tics; • head movements simulating throwing off an invisible headdress; • biting and licking lips; • spitting, etc.
All these mono-disorders can be corrected and treated quite successfully, and also rarely progress.
Diagnosis of mastopathy
One of the most significant ways to timely detect breast diseases is self-examination.
It is recommended to do it monthly, on a certain day of the menstrual cycle, preferably on the 5th–6th day, when the breasts are relaxed and soft. The procedure also involves regular examination of the underwear, shape and skin of the organ in front of the mirror. It is more comfortable to palpate the mammary glands while standing during water procedures with soapy hands or in the room using cream or lotion. It is carried out with the pads of 3-4 fingers closed together, in a circular penetrating motion. An important part of the self-examination is to feel the organ while lying on your back, one by one in each square or in a spiral direction from the outside to the nipple. The arm of the same side must be extended along the body or placed under the head. Finally, the nipple is examined, after which it must be gently squeezed between the thumb and forefinger to ensure that there is no discharge.
Three specialists are involved in the diagnosis and treatment of mastopathy: a gynecologist, a gynecologist-endocrinologist and a mammologist. To detect diffuse pathological changes in organ tissue, determine the shape, size, and number of formations, instrumental examination methods are used:
- X-ray examination of the mammary glands - mammography. The method is one of the most informative and specific; it involves taking a picture of the breast in two projections. Performed mainly in the first phase of the menstrual cycle.
- Ultrasound. Indicated for all women under 40 years of age, from 40 years of age mammography is required, and ultrasound is preferably once a year.
- Ductography. A contrast agent is injected into the mammary gland through the nipple and X-rays are taken. This is how the milk duct system is studied.
- Digital tomosynthesis. Recommended for equivocal mammography results. Layer-by-layer images of the mammary glands are reconstructed by a computer program into a three-dimensional image, which allows a more detailed examination of all the structures of the organ.
- MRI.
Note that all findings on ultrasound, mammography and/or MRI are assessed according to BI-RADS criteria - a scoring system for assessing the risk of breast cancer.
If cancer is suspected, the doctor prescribes a fine-needle aspiration biopsy of the mammary gland and a cytological examination of nipple discharge.
To determine the hormonal levels in the body during mastopathy, laboratory tests of sex hormones and instrumental examination of the organs of the endocrine system are carried out:
- blood test for prolactin, progesterone, estradiol, thyroid hormones, follicle-stimulating and luteinizing hormones;
- determination of tumor markers for the mammary gland;
- Ultrasound of internal organs;
- radiography of the sella turcica;
- CT scan of the pituitary gland.
What is the differential diagnosis of OCD?
Differential diagnosis makes it possible to distinguish OCD from a number of other mental disorders, which are also characterized by obsessions and ritualistic actions. OCD in the case of obsessive thoughts of perverted content, as well as eccentric, increasingly complex and expanding rituals must be differentiated from sluggish schizophrenia. The presence of prolonged obsessive states must be distinguished from paroxysmal schizophrenia. The possibility of schizophrenia may be indicated by sharply increasing anxiety, the inclusion of new objects in the sphere of obsessive associations, when objects, situations or accidentally spoken words that were previously indifferent to the patient remind him of phobias and take on a threatening meaning. Sometimes it is necessary to differentiate OCD with habitual tics from Gilles de la Tourette syndrome with generalization of tics, when the latter are localized in the face, neck, limbs and are expressed by grimacing, protruding the tongue, sharp and strong gestures. In addition, it is necessary to differentiate between OCD and depressive disorder. This is due to the fact that they often accompany each other. In the acute phase, the disorder whose symptoms predominate is usually diagnosed. When the process becomes chronic, a diagnosis is made of the disorder whose symptoms persist when the symptoms of another disappear.
ICD-10 notes that the differential diagnosis between obsessive-compulsive disorder and depressive disorder (F32, F33) can be difficult because the two types of symptoms often occur together. In an acute episode, preference is given to the disorder whose symptoms occurred first. When both are present but neither is dominant, it is recommended to assume that the depression was primary. For chronic disorders, it is recommended to give preference to the disorder whose symptoms persist most often in the absence of symptoms of the other.
The principle of palpation for pancreatitis
This method has been used since the mid-20th century, when it was not possible to use special equipment for diagnostics; doctors trusted their fingers during examination. And now palpation and percussion are included in the research complex for making a diagnosis.
In a healthy person, the pancreas cannot be palpated. The only thing that will help is excellent knowledge of the anatomical structure of the human body. You can feel the pulsation of the aorta on the anterior abdominal wall during examination, a large vascular trunk lying on the spine. When palpating and percussing the pancreas, it is necessary to observe changes in the nature of the patient's pain.
What are the features of the course of OCD?
A feature of the course of OCD is the chronicity of the pathological process. The transition to isolated episodes and complete recovery are extremely rare, but a relative positive is that with properly organized treatment, as well as in mild forms of OCD, long-term stabilization of the process and mitigation of symptoms can be achieved, which allows the patient to once again adapt to life in society. Severe and complicated forms of OCD in the form of various phobias can be persistent, difficult to treat, and often recurrent.
Pancreatic zones
With the help of palpation, painful areas of the pancreas can be detected. They are divided into three types:
- Shoffara (located between the navel and the armpit on the right).
- Janovera (located along the horizontal line of the navel and 4 cm to the left of it).
- Gubergritsa-Skulsky (located like the Shoffar zone, only on the left).
Thanks to the examination, you can get a preliminary picture of the disease. When examined by other methods, it is easy to make a correct diagnosis and prescribe effective treatment.
How to treat obsessive-compulsive disorder?
Obsessive-compulsive disorder, the treatment of which depends on the nature of the course, clinical picture, symptoms and mental characteristics of the patient, has common principles in organizing therapy. This is, first of all, a comprehensive treatment that combines the following main areas: • Drug therapy, which is selected strictly individually, taking into account the characteristics of OCD symptoms, gender, age, and the presence of concomitant diseases. Pharmacotherapy for OCD uses tranquilizers, SSRI antidepressants, MAO inhibitors, beta blockers to relieve autonomic symptoms, as well as antipsychotics. Therefore, self-medication is categorically excluded, because only a psychiatric specialist can assess all the risks and effectiveness of using certain drugs, develop a competent treatment regimen and prescribe the correct dosage. What is the difference between a psychotherapist and a psychiatrist. • Psychotherapy, the main goal of which is to instill in the patient faith in the success of treatment, overcome his fears about the prescribed psychotropic drugs, and convince him of the need to strictly follow the treatment regimen developed by the doctor. All this can be achieved only on the basis of a trusting relationship between the doctor and the patient and with the active support of the patient from his relatives. If the patient has ritual actions, such a method of psychotherapy as creating conditions for aggravating the situation while simultaneously blocking the reaction to what is happening is quite effective. As a result, rituals become less pronounced, and with their “depreciation,” obsessive thoughts go away. When treating panphobia, behavioral psychotherapy has a good effect, but it should be borne in mind that it is ineffective in treating obsessive “non-ritual” thoughts that are not accompanied by rituals.
In the first stages of treatment for OCD, the patient should be explained the nature of the symptoms that are disturbing him, reassure him that he is not going crazy (patients with OCD are quite often convinced of this) and establish psycho-emotional contact with him. It is important to enlist the support of the patient’s relatives, who should not indulge his obsessions, but at the same time be sympathetic to his condition and try to soften the psychological situation.
It should be noted that psychotherapy, for all its importance, cannot replace drug treatment. Explanatory and educational psychotherapy alone may be counterproductive, as in some cases it leads to an increase in the intensity of negative thoughts about the topics discussed. Only complex treatment is most effective, and long-term use of pharmacological drugs is necessary to prevent relapses.
As for prognosis, 2/3 of OCD patients experience improvement after treatment for a year, towards the end of this period. If improvement occurs after 1 year, then during the course of the disease there is an alternation of periods of remissions and exacerbations. In especially severe, advanced and complex cases, OCD symptoms turn out to be extremely resistant to treatment and do not change even after 13-20 years of illness. Timely seeking psychiatric help allows you to achieve stable and long-term remission that lasts for years. This is why knowledge of the main signs of OCD is so important - their early detection in yourself or loved ones should alert you and force you to seek help from specialists as quickly as possible.
How does the Mayo Robson sign manifest itself?
Pain when pressing on the Mayo Robson point appears with the development of acute pancreatitis. It is worth noting that the method only works in 45% of cases.
How to find the right point?
When pressing on the Mayo Robson point, a patient with pancreatitis feels a sharp, severe pain. The diagnostic method is based on this. But to use it, the doctor must correctly determine the location of the point:
- first you need to determine point A, it is located in the middle of the lowest left edge;
- point B is located in the navel area;
- an imaginary line connects points A and B;
- the line is mentally divided into 3 parts;
- the point located on the border between parts 2 and 3 is the desired one.
If the tail of the gland is affected, the pain will radiate to the back or abdominal wall. For other organ lesions, the method will not be informative.